Endoscopic Diagnosis
Gastroscopy and Colonoscopy
Gastroscopy is the most commonly used and accurate method for examining diseases of the esophagus, stomach, and duodenum, while colonoscopy is primarily used to observe pathological changes in the entire colon and rectum, from the anus to the ileocecal valve. Endoscopic examination allows direct visualization of mucosal lesions and enables biopsy sampling. With continuous advancements in endoscopic equipment, techniques such as chromoendoscopy, magnification endoscopy, narrow-band imaging, and confocal endoscopy have been incorporated, significantly improving the detection rate of early-stage tumors.

Figure 1 Gastroscopy and Colonoscopy
1, Esophagus
2, Dentate line of the cardia
3, Gastric antrum and pylorus
4, Gastric angle
5, Gastric fundus
6, Duodenal bulb
7, Descending part of the duodenum
A, Rectum
B, Ileocecal region
During gastroscopy or colonoscopy, patients can be administered appropriate doses of fast-acting sedatives and anesthetics intravenously under strict monitoring. This reduces discomfort such as nausea, emesis, or agitation during the procedure, facilitating patient cooperation. It also reduces oral secretions and gastrointestinal peristalsis, which aids in lesion observation and biopsy. After the procedure, patients typically experience no discomfort upon waking.
Under direct endoscopic visualization, various bleeding lesions can be treated for hemostasis, foreign bodies in the stomach can be removed, and smaller or pedunculated polyps and benign tumors can be completely excised using techniques such as snaring, electrocautery, or argon plasma coagulation. For larger benign tumors and early-stage cancers, endoscopic mucosal resection (EMR) or submucosal dissection (ESD) can be performed as needed. Endoscopic treatment has reduced the need for conventional open surgeries, making interventions more precise and minimally invasive. This approach helps reduce complications, medical costs, and hospital stays.
Capsule Endoscopy
Capsule endoscopy consists of a capsule, a signal-receiving system, and a workstation. During the examination, the patient swallows a capsule equipped with a miniature camera, which captures images of the gastrointestinal tract at a rate of 2 frames per second as it moves through the digestive system. These images are transmitted to the signal-receiving system and later analyzed on the workstation. Capsule endoscopy provides dynamic and clear visualization of lesions within the small intestine, overcoming the limitations of conventional small intestine examinations. Its advantages include being painless and safe, making it the first-line diagnostic method for suspected small intestine diseases.
Enteroscopy
Unlike capsule endoscopy, enteroscopy has suction and insufflation functions, allowing clearer observation of lesions. It also enables biopsy sampling and endoscopic treatment of detected lesions. However, enteroscopy is limited in its ability to examine the entire small intestine and has a lower positive detection rate for small intestine lesions compared to capsule endoscopy. Additionally, the procedure is time-consuming and causes more discomfort for patients. Therefore, enteroscopy is typically used after capsule endoscopy has identified small intestine lesions that require further direct examination, biopsy, or endoscopic treatment.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP involves inserting a catheter into the common bile duct or pancreatic duct through the duodenal papilla under direct visualization with a duodenoscope. Contrast agents are then injected retrograde, and X-ray imaging is used to visualize the anatomy of the biliary and pancreatic ducts. In addition to its diagnostic applications, ERCP is now more commonly used for therapeutic purposes in biliary and pancreatic diseases. Therapeutic ERCP includes endoscopic sphincterotomy, stone extraction from the common bile duct, dilation of strictures, stent placement, and nasobiliary drainage. Its minimally invasive, effective, and repeatable nature has reduced the need for conventional surgical interventions.
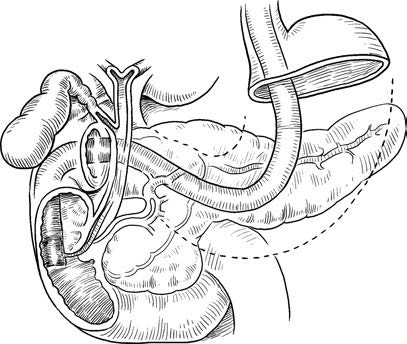
Figure 2 ERCP
Endoscopic Ultrasonography (EUS)
EUS combines endoscopy with ultrasonography by placing a miniature high-frequency ultrasound probe at the tip of the endoscope or inserting it through the endoscopic channel. This allows simultaneous direct visualization of intraluminal lesions and real-time ultrasound scanning to assess the origin of lesions within specific layers of the gastrointestinal wall and the condition of adjacent organs. Compared to surface ultrasonography, EUS eliminates or shortens the distance between the ultrasound source and the target organ, reducing sound attenuation and avoiding interference from bones, fat, or gas-containing structures. This results in the clearest possible echo imaging.
Under EUS guidance, procedures such as lesion biopsy, tumor intervention, cyst drainage, and celiac plexus neurolysis can be performed.
Laboratory Tests
Diagnosis of Hepatitis B Virus Infection
The diagnosis of hepatitis B virus (HBV) infection includes the detection of five serological immune markers (HBsAg, HBsAb, HBeAg, HBeAb, and HBcAb), serum viral tests (quantitative HBV-DNA, HBV genotyping, and detection of HBV drug-resistant mutations), and tissue virological tests (HBsAg, HBcAg, and HBV-DNA in liver tissue).
The five commonly used serological immune markers of HBV help determine whether a patient is infected with HBV. Quantitative HBV-DNA testing reflects the level of viral replication. These two tests are often used to decide whether antiviral therapy is necessary and to evaluate treatment efficacy.
Helicobacter pylori Detection
Helicobacter pylori (Hp) detection plays an important role in the diagnosis and treatment of diseases such as precancerous gastric conditions, peptic ulcers, and mucosa-associated lymphoid tissue (MALT) lymphoma.
Non-invasive methods
The commonly used 13C- or 14C-urea breath test (Hp-UBT) does not rely on endoscopy, offers good patient compliance, and has high accuracy, making it one of the most important methods for Hp detection. It is widely used in hospitals. However, Hp-UBT has certain limitations, as its results can be affected by antibiotics, bismuth-containing agents, and acid-suppressing medications. The detection of Hp antigens in stool using monoclonal antibody enzyme-linked immunosorbent assay (ELISA) is a simple and convenient method with sensitivity and accuracy comparable to Hp-UBT. However, its clinical application is currently less widespread than the breath test.
Invasive methods
These include rapid urease tests, histological examination of gastric mucosal biopsies (e.g., Warthin-Starry silver staining), and bacterial culture. Gastric mucosal biopsy for bacterial culture is generally not used for routine clinical diagnosis and is primarily employed in research settings.
Liver Function Assessment
Liver Synthetic Function
Serum albumin
Albumin is synthesized exclusively by hepatocytes. A significant reduction in serum albumin levels indicates impaired liver synthetic function. In stable conditions, serum albumin levels may remain within the normal range in some patients. However, after events such as bleeding, infection, or surgery, serum albumin levels may decrease significantly and may not return to normal.
Plasma coagulation factors
Most coagulation factors are synthesized in the liver, with half-lives much shorter than that of albumin, particularly vitamin K-dependent factors (II, VII, IX, and X). In the early stages of liver dysfunction, coagulation factors may decrease significantly even when albumin levels are still normal. Commonly used indicators include prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time (TT).
Cholesterol
Approximately 70% of endogenous cholesterol is synthesized in the liver. Liver dysfunction can lead to reduced blood cholesterol levels.
Hepatocellular Injury
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are present in the cytoplasm of hepatocytes. When the hepatocyte membrane is damaged, ALT and AST levels rise significantly, making them important indicators of hepatocellular injury. Since AST is also present in tissues such as skeletal muscle, kidneys, and myocardium, a predominant elevation of AST in the blood does not necessarily indicate liver injury. AST is mainly located in mitochondria within hepatocytes. When both ALT and AST levels are elevated, with AST showing a marked increase, this suggests severe hepatocellular damage. In severe hepatitis, a decline in transaminase levels accompanied by elevated bilirubin levels (a phenomenon known as "enzyme-bilirubin dissociation") indicates extensive hepatocyte necrosis and is associated with a mortality rate of approximately 90%. In chronic liver diseases, ALT and AST levels are often mildly to moderately elevated. In liver cirrhosis, where fibrosis and hepatocyte atrophy predominate, ALT and AST levels may remain normal in many patients.
Bilirubin Metabolism
Bilirubin is a product of the breakdown of aging red blood cells by the mononuclear phagocyte system in the liver, spleen, and bone marrow. Total bilirubin (TB) consists of unconjugated bilirubin (UCB) and conjugated bilirubin (CB). Unconjugated bilirubin is a metabolic product of hemoglobin, which is taken up by hepatocytes and converted into water-soluble conjugated bilirubin for excretion via the bile ducts. Obstruction at any stage of this process can lead to jaundice. Serum bilirubin testing helps detect subclinical jaundice and often reflects hepatocellular injury or bile stasis. The presence of bilirubin in urine suggests elevated serum conjugated bilirubin levels. When the liver cannot process urobilinogen reabsorbed from the intestine, urinary urobilinogen levels increase.
Since liver function indicators do not fully correlate with liver health, comprehensive assessments should combine symptoms, physical signs, imaging data, and pathology. When liver damage and dysfunction are confirmed, identifying the underlying causes is essential. The Child-Pugh score is often used to grade liver function for clinical decision-making. As liver function grades can fluctuate with disease progression, a flexible approach is recommended.
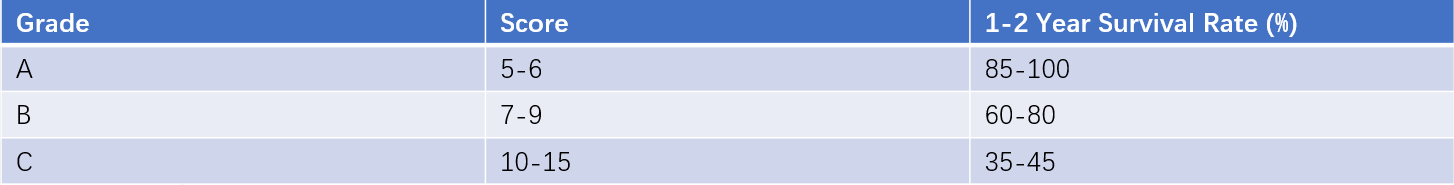
Table 1 Child-Pugh scoring for liver function
Analysis of Exocrine Pancreatic Function
This involves measuring various digestive enzymes secreted by the pancreas. Functional tests are categorized as direct or indirect. Direct tests involve collecting pancreatic secretions after intravenous injection of secretagogues or a combination of secretagogues. Indirect tests stimulate pancreatic secretion through test meals and measure the breakdown products of pancreatic enzymes to evaluate exocrine pancreatic function indirectly.
Autoimmune Diseases
This includes testing for parietal cell antibodies, intrinsic factor antibodies, pepsinogen I/II levels, and various other autoantibodies associated with autoimmune gastritis.
Microbial Testing
This includes detecting and culturing microorganisms in blood, stool, urine, and peritoneal fluid, as well as analyzing antibodies produced by microorganisms.
Tumor Markers for Digestive System Cancers
Common tumor markers for digestive system cancers include alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA), CA19-9, and CA72-4.
Imaging Diagnosis
Ultrasound
Ultrasound is widely used in clinical practice to examine solid organs of the digestive system, the biliary tract, and intra-abdominal lesions. Its advantages include being non-invasive, radiation-free, cost-effective, convenient, rapid, and capable of assessing hemodynamic parameters. However, its diagnostic capability is limited for tissues or organs obscured by gas or bone, and its accuracy is significantly influenced by the operator's skill and experience.
CT
Contrast-enhanced CT scanning is an essential diagnostic tool for detecting small lesions, isodense lesions, lesions requiring localization and characterization, and vascular abnormalities in the digestive system. Advances in CT scanning speed, resolution, more powerful post-processing software, efficient image review methods, and the gradual reduction in costs have greatly enhanced its role in diagnosing abdominal diseases. However, caution is required in patients with impaired liver or kidney function, and its use may be contraindicated in such cases.
MRI
MRI is suitable for observing small lesions and for the qualitative diagnosis of abnormalities. It is particularly valuable for differentiating the histological origin of lesions in the liver hilum and for diagnosing biliary and pancreatic diseases. Magnetic resonance cholangiopancreatography (MRCP), a non-invasive imaging technique based on water imaging principles, provides a clear visualization of the entire lumen of fluid-filled bile ducts and pancreatic ducts without the need for contrast agent injection. It is an important diagnostic method for biliary and pancreatic diseases.