Hypothyroidism, or underactive thyroid, is a systemic low metabolic syndrome caused by reduced synthesis and secretion of thyroid hormones or insufficient utilization by peripheral tissues due to various factors. The prevalence of clinical hypothyroidism is approximately 0.3%–1.0%, while subclinical hypothyroidism occurs in about 4% of the population. The prevalence increases with age and is higher in females than in males.
Classification
Classification based on the site of the lesion
Primary Hypothyroidism
Hypothyroidism caused by thyroid gland dysfunction accounts for over 99% of cases.
Central Hypothyroidism
Hypothyroidism results from decreased production and secretion of TRH or TSH due to hypothalamic or pituitary lesions. Hypothyroidism caused by hypothalamic dysfunction is referred to as tertiary hypothyroidism.
Thyroid Hormone Resistance Syndrome
This is a condition in which thyroid hormones fail to exert their normal biological effects in peripheral tissues. It is an autosomal dominant genetic disorder, with mutations in the thyroid hormone receptor beta (THRβ) gene being the most common cause.
Classification based on the degree of hypothyroidism
Primary hypothyroidism is further categorized into overt hypothyroidism and subclinical hypothyroidism.
Etiology
The causes of hypothyroidism are diverse, with autoimmune damage being the primary underlying factor, such as in autoimmune thyroiditis.
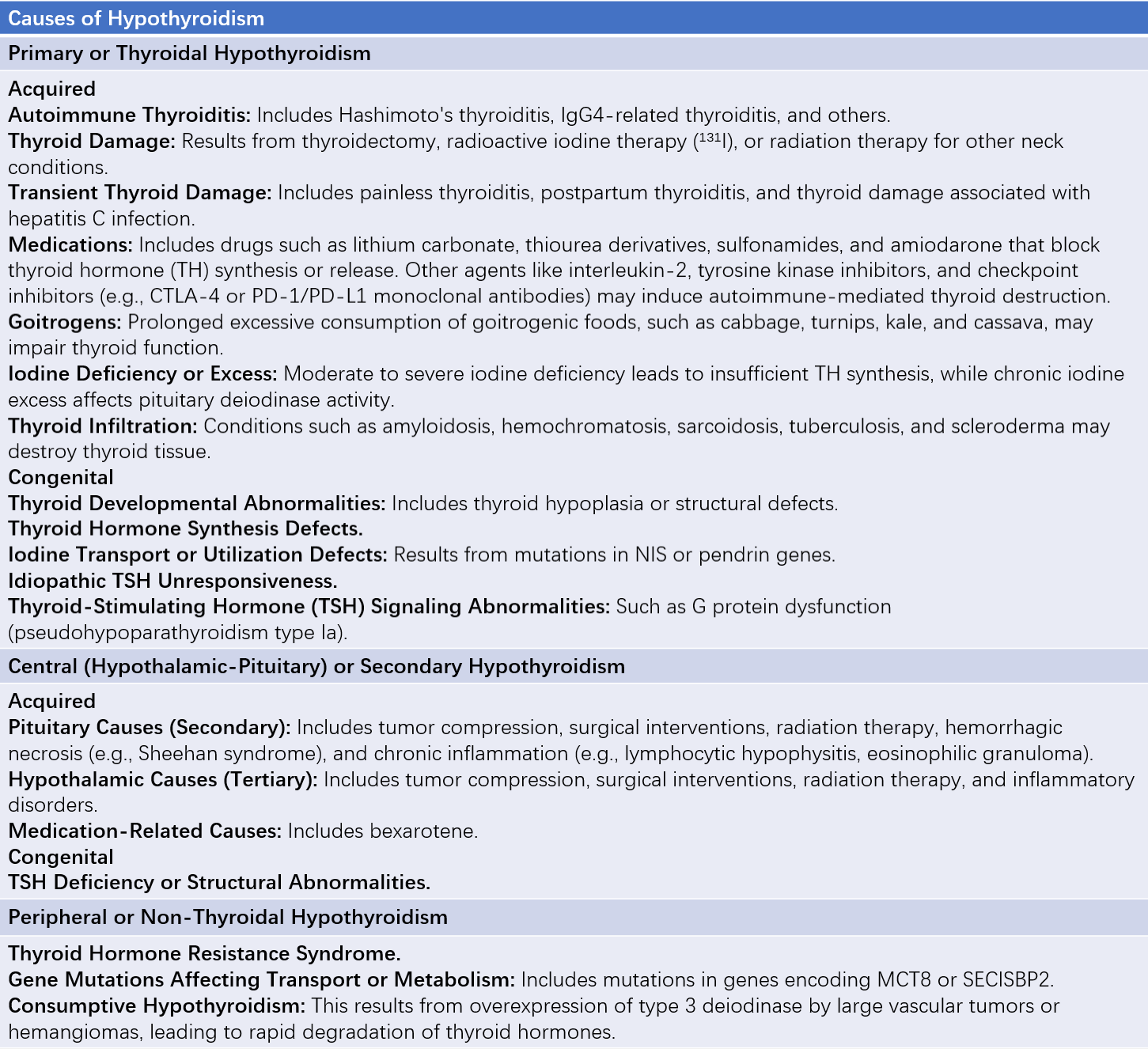
Table 1 Causes of hypothyroidism
Note:
CTLA-4: Cytotoxic T lymphocyte-associated antigen-4.
PD-1/PD-L1: Programmed cell death protein 1/PD-1 ligand.
TH: Thyroid hormone.
NIS: Sodium-iodide symporter.
MCT8: Monocarboxylate transporter 8.
SECISBP2: Selenocysteine insertion sequence-binding protein 2.
Pathology
Thyroid pathology varies based on the underlying cause. For instance, in chronic lymphocytic thyroiditis, massive infiltration of lymphocytes and plasma cells occurs, leading to follicle destruction, replacement by fibrotic tissue, follicular atrophy, flattened follicular cells, and colloid-filled lumens. In primary hypothyroidism, reduced thyroid hormones weaken the feedback inhibition on the pituitary, leading to TSH cell hyperplasia and even the development of TSH-secreting adenomas. In hypothyroid patients, hyaluronic acid and chondroitin sulfate B mucopolysaccharide deposits are present in the skin and connective tissues, which stains positively with PAS, causing myxedematous changes.
Clinical Manifestations
Medical History
A detailed medical history is helpful for diagnosis. Relevant details may include a history of thyroid surgery, radioiodine therapy for hyperthyroidism, Graves' disease, Hashimoto's thyroiditis, or prior medication usage.
Clinical Symptoms
The onset of hypothyroidism is insidious, and the disease course is relatively long. Clinical symptoms are primarily characterized by reduced basal metabolic rate and decreased sympathetic nervous excitability. Mild or early-stage patients may have nonspecific symptoms. Typical symptoms include fatigue, cold intolerance, decreased sweating, swelling in the hands or feet, weight gain, drowsiness, memory loss, joint pain, constipation, menstrual irregularities (increased flow, irregular cycles, or infertility in women), and galactorrhea. In males, hypothyroidism may result in reduced libido, erectile dysfunction, or decreased sperm count.
Myxedematous coma represents the most severe form of hypothyroidism. It is more commonly seen in elderly individuals or those with long-standing untreated disease, typically triggered by cold weather. Precipitating factors include acute systemic illnesses, abrupt discontinuation of thyroid hormone therapy, infections, surgeries, anesthetics, or sedative medications. Clinical signs include drowsiness, hypothermia (<35°C), slowed respiration, bradycardia, hypotension, muscle flaccidity, diminished or absent reflexes, and in severe cases, coma or shock. Life-threatening complications such as heart or kidney failure may occur.
Physical Examination
Typical findings include dull facial expressions, slow reactions, hoarseness, hearing impairments, and pale complexion. Myxedematous facies are characterized by non-pitting swelling of the face and/or eyelids, along with an expressionless, apathetic appearance resembling a "mask-like" face. The nose and lips appear thickened, the tongue is enlarged, and speech may become slurred. The skin is dry, coarse, cool to touch, and scaly, with hair that is dry, brittle, and sparse. The lateral one-third of the eyebrows may be absent, and nails may appear thickened and brittle. Palms and soles may exhibit a yellowish hue due to hypercarotenemia. Other common findings include a slowed heart rate and prolonged Achilles tendon reflex time.
Laboratory Tests
Serum TSH, TT4, and FT4
A reduction in FT4 or TT4 serves as a key criterion for diagnosing overt hypothyroidism. In primary hypothyroidism, elevated TSH occurs before a reduction in T4, making serum TSH the most sensitive marker for evaluating primary hypothyroidism.
TRH Stimulation Test
This test helps differentiate the causes of hypothyroidism. A lack of increase in serum TSH following intravenous administration of TRH suggests pituitary hypothyroidism. A delayed increase indicates hypothalamic hypothyroidism. An elevated baseline TSH level with a further exaggerated increase after TRH stimulation suggests primary hypothyroidism.
Serum TPOAb and TgAb
Positive serum thyroid peroxidase antibody (TPOAb) or thyroglobulin antibody (TgAb) indicates that hypothyroidism is caused by autoimmune thyroiditis. TPOAb positivity is generally considered to have stronger diagnostic significance.
Other Tests
Mild to moderate anemia may be observed. Increases in serum total cholesterol and cardiac enzymes can occur. In some cases, elevated serum prolactin levels and pituitary enlargement may be present. Genetic testing can clarify the etiology when hereditary hypothyroidism is strongly suspected.
Diagnosis
Primary Hypothyroidism
Elevated serum TSH with reduced FT4 and/or TT4 levels confirms the diagnosis. Severe cases may also show reduced FT3 and/or TT3 levels.
Subclinical Hypothyroidism
Elevated serum TSH with normal FT4 and TT4 levels indicates subclinical hypothyroidism. Positivity for TPOAb or TgAb suggests autoimmune thyroiditis as the underlying cause.
Central Hypothyroidism
Reduced or normal serum TSH, along with decreased FT4 and/or TT4 levels, suggests central hypothyroidism. Further investigation should identify pituitary or hypothalamic pathology.
Differential Diagnosis
Anemia
Differentiation from other causes of anemia is necessary. Hypothyroidism and pernicious anemia share several clinical and immunological similarities. Thyroid function tests clarify the distinction.
Edema
Edema associated with chronic nephritis or nephrotic syndrome can present with reduced TT3 and TT4 levels and increased cholesterol levels. However, abnormal renal function coupled with TSH and FT4/FT3 testing aids in differentiation.
Euthyroid Sick Syndrome (ESS)
Also known as low T3 syndrome, ESS is a protective response of the body to severe chronic illnesses unrelated to thyroid dysfunction. Serum T3 levels are reduced, and in severe cases, T4 levels may also decrease. Elevated reverse triiodothyronine (rT3) is observed in ESS. The mechanisms involve:
- Inhibition of 5'-deiodinase activity, reducing peripheral conversion of T4 to T3 and consequently lowering T3 levels.
- Activation of inner-ring deiodination of T4, converting T4 to rT3, leading to rT3 elevation.
Differentiating ESS from central hypothyroidism is challenging; a decreased rT3 level in central hypothyroidism may help in differentiation.
Enlarged Sella Turcica
Differentiation from pituitary tumors is necessary. In primary hypothyroidism, increased TRH secretion can lead to hyperprolactinemia, galactorrhea, and enlargement of the sella turcica, mimicking pituitary prolactinoma.
Pericardial Effusion
Differentiation from other causes of pericardial effusion is required. Pericardial effusion caused solely by hypothyroidism can resolve with thyroxine therapy.
Treatment
Thyroid Hormone Replacement Therapy
Levothyroxine (L-T4) monotherapy is the preferred treatment. The goal of therapy is to restore serum TSH and thyroid hormone levels to their normal range, and lifelong medication is typically required. The appropriate dosage depends on the patient's condition, etiology, age, and body weight and should be individualized. For clinical hypothyroidism, the replacement dose for adults is typically 1.6–1.8 μg/(kg·d). In elderly patients, the dose is lower, approximately 1.0 μg/(kg·d). During pregnancy, the dose is generally increased by 30%–50%. For subclinical hypothyroidism, the L-T4 dose is determined based on TSH levels. The initial dose of L-T4 and the time required to achieve the full replacement dose depend on the patient’s age, cardiac status, and other specific factors. In patients with ischemic heart disease, the starting dose should be low, and dosage adjustments should be made gradually to avoid exacerbating or triggering heart conditions.
L-T4 has a half-life of 7 days, making once-daily dosing sufficient. Desiccated thyroid preparations derived from animal thyroid glands are rarely used due to unstable thyroid hormone content and excessive T3 levels. Liothyronine (L-T3) acts quickly but has a shorter duration of action, making it suitable for emergencies like myxedematous coma. Re-establishing the balance of the hypothalamic-pituitary-thyroid axis through thyroid hormone supplementation generally takes 4–6 weeks. Hormone levels, including TSH and T4, are typically monitored every 4–6 weeks at the beginning of treatment. Once stabilized, follow-up tests are recommended every 6–12 months. For central hypothyroidism, dosage adjustments rely on FT4 levels rather than TSH.
General Treatment
For patients with anemia, iron supplements, vitamin B12, or folic acid may be provided. In cases of iodine deficiency, iodized salt consumption or iodine supplementation is recommended.
Treatment of Myxedematous Coma
Thyroid Hormone Supplementation
Intravenous levothyroxine (L-T4) or liothyronine (L-T3) is the first-line treatment. L-T3 is typically administered intravenously. If intravenous formulations are unavailable, L-T3 tablets can be administered via a nasogastric tube. Alternately, an initial intravenous dose of L-T4 of 200–400 μg can be given, followed by daily intravenous dosing of 1.6 μg/kg, or L-T4 can be given via nasogastric tube until the patient regains consciousness, at which point oral administration can be initiated.
Supportive Measures
Ensuring adequate warmth, providing oxygen therapy, and maintaining airway patency are crucial. Tracheotomy or mechanical ventilation may be utilized if necessary.
Glucocorticoid Therapy
Hydrocortisone at a dose of 200–400 mg/day can be administered via continuous intravenous infusion, with gradual tapering once the patient regains consciousness.
Fluid, Electrolyte, and Acid-Base Balance
Intravenous fluid therapy is administered as needed, but excessive fluid intake should be avoided.
Infection Control and Management of Underlying Conditions
Antibiotics or other treatments may be used to address infections or primary diseases. Supportive measures and enhanced nursing care are also important components of management.