Cor pulmonale, commonly referred to as pulmonary heart disease, is defined as a condition caused by bronchopulmonary, thoracic, or pulmonary vascular lesions that lead to increased pulmonary vascular resistance, resulting in pulmonary hypertension and subsequent structural and/or functional changes in the right ventricle. Based on the onset and duration of the disease, it can be classified into acute and chronic cor pulmonale. Acute cor pulmonale is often associated with acute massive pulmonary embolism, which is discussed in pulmonary embolism. This section focuses on chronic cor pulmonale.
Etiology
Based on the location of the primary disease, chronic cor pulmonale can be classified into the following categories:
Bronchopulmonary Diseases
Chronic obstructive pulmonary disease (COPD) is the most common cause, accounting for approximately 80%-90% of cases. Other causes include interstitial lung disease, bronchial asthma, bronchiectasis, and pulmonary tuberculosis.
Thoracic Movement Disorders
These are relatively rare and include severe thoracic or spinal deformities and neuromuscular diseases, which can restrict thoracic activity, compress the lungs, and cause bronchial distortion or deformation, leading to impaired lung function. Impaired airway drainage, recurrent pulmonary infections, and complications such as emphysema or fibrosis may occur.
Pulmonary Vascular Diseases
Idiopathic pulmonary arterial hypertension, chronic thromboembolic pulmonary hypertension (CTEPH), and pulmonary arteritis can all increase pulmonary vascular resistance, elevate pulmonary arterial pressure, and overload the right ventricle, eventually leading to chronic cor pulmonale.
Other Causes
Primary alveolar hypoventilation, congenital oropharyngeal malformations, and obstructive sleep apnea can all result in hypoxemia, causing pulmonary vasoconstriction and pulmonary hypertension, which may progress to chronic cor pulmonale.
Pathogenesis and Pathophysiology
Development of Pulmonary Hypertension
Pulmonary vasoconstriction plays a key role in the development of hypoxic pulmonary hypertension. Hypoxia, hypercapnia, and respiratory acidosis cause pulmonary vasoconstriction and spasm, with hypoxia being the most critical factor in the development of pulmonary hypertension.
During hypoxia, the production of vasoconstrictive substances such as leukotrienes, serotonin (5-HT), angiotensin II, and platelet-activating factor (PAF) increases, leading to pulmonary vasoconstriction and elevated vascular resistance. The imbalance between endothelium-derived relaxing factors (EDRF) and endothelium-derived contracting factors (EDCF) also contributes to hypoxic pulmonary vasoconstriction. Hypoxia increases the permeability of smooth muscle cell membranes to Ca2+, raising intracellular Ca2+ levels, which enhances the excitation-contraction coupling of muscles and directly induces pulmonary vascular smooth muscle contraction.
Hypercapnia, due to excessive H+ production, increases the sensitivity of blood vessels to hypoxic contraction, further raising pulmonary arterial pressure.
Anatomical factors refer to structural changes in the pulmonary vasculature, resulting in hemodynamic disturbances in pulmonary circulation. The main causes include:
- Pulmonary vascular remodeling: Common causes include pulmonary arterial lesions in idiopathic pulmonary hypertension and chronic thrombotic obstruction in CTEPH. Chronic hypoxia in diseases like COPD and interstitial lung disease induces pulmonary vasoconstriction, increasing vascular wall tension. Additionally, hypoxia stimulates the production of various growth factors (e.g., polypeptide growth factors) in the lungs, directly promoting the proliferation of smooth muscle cells, elastic fibers, and collagen fibers in the vascular wall.
- Chronic inflammation: Recurrent exacerbations of COPD and peribronchial inflammation may involve adjacent pulmonary arterioles, causing vasculitis, vascular wall thickening, luminal narrowing, or fibrosis, and even complete occlusion, thereby increasing pulmonary vascular resistance and leading to pulmonary hypertension.
- Emphysema: Alveolar overinflation in emphysema increases intrapulmonary pressure, compressing alveolar capillaries and narrowing or occluding their lumens. Alveolar wall rupture destroys the capillary network, and when the loss of the alveolar-capillary bed exceeds 70%, pulmonary vascular resistance increases.
- Thrombosis: Autopsy findings reveal that some patients with acute exacerbations of chronic cor pulmonale have multiple in situ thrombi in small pulmonary arterioles, which increase pulmonary vascular resistance and exacerbate pulmonary hypertension.
Chronic hypoxia induces secondary polycythemia, increasing blood viscosity. Hypoxia also elevates aldosterone levels, causing water and sodium retention. Additionally, hypoxia induces renal arteriole constriction, reducing renal blood flow and further aggravating water and sodium retention, leading to increased blood volume. Both increased blood viscosity and blood volume contribute to elevated pulmonary arterial pressure.
Cardiac Changes and Heart Failure
Increased pulmonary vascular resistance leads to pulmonary hypertension, prompting compensatory hypertrophy of the right ventricle to overcome the elevated pulmonary arterial resistance. In the early stages of pulmonary hypertension, the right ventricle can still compensate, and end-diastolic pressure remains normal. As the disease progresses, particularly during acute exacerbations, persistently elevated pulmonary arterial pressure exceeds the compensatory capacity of the right ventricle, resulting in right ventricular decompensation. This leads to reduced right ventricular output, increased residual blood volume at the end of systole, elevated end-diastolic pressure, right ventricular dilation, and right heart failure.
Damage to Other Vital Organs
Hypoxia and hypercapnia, in addition to affecting the heart, also cause pathological changes in other vital organs such as the brain, liver, kidneys, gastrointestinal tract, endocrine system, and hematological system, resulting in multi-organ dysfunction.
Clinical Manifestations
Compensated Stage of Pulmonary and Cardiac Function
Patients may present with cough, expectoration, and shortness of breath. Palpitations, dyspnea, fatigue, and reduced exercise tolerance may occur after physical activity. Chest pain or hemoptysis is rare.
Cyanosis of varying degrees may be observed, along with signs of the underlying pulmonary disease, such as emphysema, dry or moist rales, and an accentuated pulmonary component of the second heart sound (P2 > A2). A systolic murmur in the tricuspid valve area or increased cardiac pulsations below the xiphoid process may indicate right ventricular hypertrophy. In some patients, elevated intrathoracic pressure due to emphysema may impair venous return, leading to distended or engorged neck veins. The diaphragm may also be displaced downward, resulting in a lower liver border.
Decompensated Stage of Pulmonary and Cardiac Function
Respiratory Failure
Worsening dyspnea is commonly reported, along with headache, insomnia, anorexia, and daytime drowsiness. Some patients may exhibit symptoms of pulmonary encephalopathy, such as apathy, confusion, or delirium.
Severe cyanosis and conjunctival congestion or edema may be present. In advanced cases, signs of increased intracranial pressure, such as retinal vessel dilation and papilledema, may occur. Tendon reflexes may be diminished or absent, and pathological reflexes may appear. Hypercapnia may lead to peripheral vasodilation, manifesting as flushed skin and excessive sweating.
Right Heart Failure
Pronounced dyspnea, palpitations, loss of appetite, abdominal distension, and nausea are common.
Severe cyanosis, engorged neck veins, tachycardia, and arrhythmias may occur. A systolic murmur may be heard below the xiphoid process, and in some cases, a diastolic murmur may also be present. The liver may be enlarged and tender, with a positive hepatojugular reflux sign. Lower extremity edema and, in severe cases, ascites may develop. Rarely, signs of pulmonary edema and global heart failure may be observed.
Auxiliary Examinations
Chest X-ray
In addition to findings related to the underlying pulmonary or thoracic disease and acute pulmonary infections, signs of pulmonary hypertension may be observed.
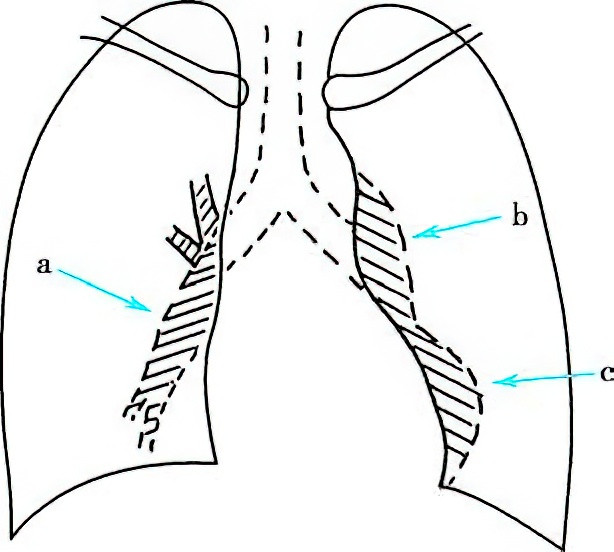
Figure 1 Frontal chest X-ray of chronic cor pulmonale
The right lower pulmonary artery trunk is widened (a), the pulmonary artery segment is prominent (b), and the cardiac apex is elevated (c).
Electrocardiography (ECG)
The diagnostic sensitivity of ECG for chronic cor pulmonale ranges from 60.1% to 88.2%. Diagnostic criteria for chronic cor pulmonale on ECG include:
- Mean frontal plane QRS axis ≥ +90°
- R/S ratio ≥ 1 in lead V1
- Severe clockwise rotation (R/S ratio ≤ 1 in lead V5)
- RV1+SV5≥1.05mVR
- R/S or R/Q ratio ≥ 1 in lead aVR
- QS, Qr, or qr patterns in leads V1-V3 (similar to myocardial infarction, requiring differentiation)
- Pulmonary P waves
The presence of any one of these criteria supports the diagnosis.
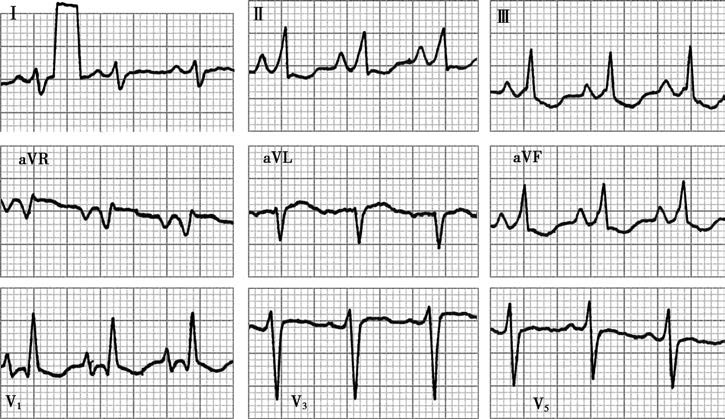
Figure 2 Electrocardiographic changes in chronic cor pulmonale
There is right axis deviation, clockwise rotation, P pulmonale, a qR pattern in the QRS complex in lead V1, R/S < 1 in lead V5, and RV1 + SV5 = 1.5 mV.
Echocardiography
The diagnostic sensitivity of echocardiography for chronic cor pulmonale ranges from 60.6% to 87.0%. Diagnostic criteria include:
- Right ventricular outflow tract diameter ≥ 30 mm
- Right ventricular diameter ≥ 20 mm
- Right ventricular anterior wall thickness ≥ 5 mm or increased anterior wall motion amplitude
- Left-to-right ventricular diameter ratio < 2
- Right pulmonary artery diameter ≥ 18 mm or pulmonary artery trunk ≥ 20 mm
- Right ventricular outflow tract to left atrial diameter ratio > 1.4
- Evidence of pulmonary hypertension on the pulmonary valve curve (e.g., a-wave < 2 mm or mid-systolic closure).
Arterial Blood Gas Analysis
Hypoxemia, respiratory failure, or hypercapnia may be present.
Blood Tests
Elevated red blood cell counts and hemoglobin levels may be observed. Whole blood and plasma viscosity may increase, and red blood cell electrophoresis time is often prolonged. In cases of cardiac dysfunction, renal or liver function abnormalities may also be present.
Other Tests
Sputum pathogen analysis can guide the selection of antibiotics. Pulmonary function tests during the early or remission stages of chronic cor pulmonale may help evaluate lung function.
Diagnosis
The diagnosis can be established based on a history of COPD, chronic bronchitis, emphysema, or other thoracic or pulmonary diseases, along with signs of elevated pulmonary arterial pressure, right ventricular enlargement, or right heart dysfunction. Clinical findings such as engorged neck veins, P2 > A2, increased cardiac pulsations below the xiphoid process, hepatomegaly with tenderness, a positive hepatojugular reflux sign, and lower extremity edema support the diagnosis. Imaging studies, including ECG, chest X-ray, and echocardiography, may reveal pulmonary artery dilation and right ventricular enlargement or hypertrophy, further confirming the diagnosis.
Differential Diagnosis
Coronary Artery Disease (CAD)
Both chronic cor pulmonale and CAD are common in older patients. CAD is often characterized by typical angina, a history of myocardial infarction, or specific ECG findings. A history of left heart failure, primary hypertension, hyperlipidemia, or diabetes is helpful for differentiation. Physical examination, chest X-ray, ECG, and echocardiography typically reveal left ventricular hypertrophy in CAD. Coronary angiography demonstrating coronary artery stenosis can confirm the diagnosis. Differentiating chronic cor pulmonale from coexisting CAD may be challenging, requiring a detailed history along with cardiac and pulmonary function tests.
Rheumatic Heart Disease (RHD)
Tricuspid valve disease in RHD should be distinguished from relative tricuspid regurgitation in chronic cor pulmonale. RHD often has a history of rheumatic arthritis or myocarditis, with involvement of other valves such as the mitral or aortic valves. X-ray, ECG, and echocardiography findings in RHD are typically distinct.
Primary Cardiomyopathy
This condition often presents with global cardiac enlargement, without a history of chronic bronchial or pulmonary disease. X-ray findings do not indicate pulmonary hypertension.
Treatment
Compensated Stage of Pulmonary and Cardiac Function
Comprehensive treatment strategies can be employed to slow the progression of underlying bronchial and pulmonary diseases, prevent infections, reduce or avoid acute exacerbations, and enhance rehabilitation and nutrition. Long-term home oxygen therapy or non-invasive ventilation may be utilized when necessary to improve the quality of life.
Decompensated Stage of Pulmonary and Cardiac Function
The treatment principles include actively controlling infections, ensuring airway patency, improving respiratory function, correcting hypoxemia and/or carbon dioxide retention, managing respiratory failure and heart failure, and preventing complications.
Infection Control
Respiratory infections are a common cause of acute exacerbations in chronic cor pulmonale, leading to decompensation of pulmonary and cardiac functions. Active infection control is required.
Management of Heart Failure
In most cases, heart failure improves after infection control, respiratory function enhancement, and correction of hypoxemia and carbon dioxide retention. Patients may show increased urine output and reduced edema without requiring routine use of diuretics or inotropic agents. However, for patients with severe heart failure or those unresponsive to the above treatments, diuretics, inotropic agents, or vasodilators may be considered.
Diuretics increase urine output by inhibiting renal sodium and water reabsorption, alleviating edema, reducing blood volume, and decreasing right heart preload. However, diuretics may cause hypokalemia, hypochloremic alkalosis, thickened sputum, and blood concentration. Mild diuretics combined with potassium-sparing diuretics are preferred, with low doses and short treatment courses. For example, hydrochlorothiazide (25 mg, 1-3 times/day) can be combined with spironolactone (20-40 mg, 1-2 times/day).
Chronic hypoxemia and infections render patients with chronic cor pulmonale more susceptible to digitalis toxicity and arrhythmias. Inotropic agents should be used cautiously and only under certain conditions:
- Persistent right heart failure despite infection control, improved respiratory function, and diuretic therapy.
- Predominant right heart failure without significant infection.
- Coexisting supraventricular tachyarrhythmias, such as supraventricular tachycardia or atrial fibrillation with a ventricular rate >100 beats/min.
- Acute left heart failure.
Fast-acting and rapidly excreted digitalis drugs are preferred, administered intravenously at reduced doses (1/2 to 2/3 of the standard dose). Common options include deslanoside (0.125-0.25 mg) or digoxin (0.2-0.4 mg) diluted in 10% glucose solution and injected slowly. Hypoxemia and hypokalemia should be corrected beforehand to prevent drug toxicity. Since hypoxemia and infections can increase heart rate, heart rate alone is not a reliable indicator for assessing the use or efficacy of digitalis drugs.
Targeted therapies may be used to reduce pulmonary vascular resistance in cases of arterial pulmonary hypertension or chronic thromboembolic pulmonary hypertension (CTEPH). However, in conditions such as COPD or interstitial lung disease-induced cor pulmonale, vasodilators may worsen ventilation-perfusion mismatch, exacerbate hypoxemia, and cause systemic arterial dilation. This can lead to systemic hypotension, reflex tachycardia, decreased oxygen partial pressure, and increased carbon dioxide partial pressure, limiting the clinical use of vasodilators.
Prevention and management of complications
Pulmonary Encephalopathy
This is a neuropsychiatric syndrome caused by hypoxemia and carbon dioxide retention due to respiratory failure, often secondary to COPD. The diagnosis requires exclusion of cerebrovascular diseases, infectious toxic encephalopathy, and severe electrolyte imbalances.
Acid-Base and Electrolyte Imbalances
Various types of acid-base and electrolyte disturbances are common during the decompensated stage of chronic cor pulmonale. Respiratory acidosis is primarily managed by ensuring airway patency, correcting hypoxemia, and relieving carbon dioxide retention. Metabolic acidosis accompanying respiratory acidosis may require bicarbonate supplementation, especially when the pH is <7.2. In such cases, 100 ml of 5% sodium bicarbonate may be administered, with further adjustments based on arterial blood gas analysis. Metabolic alkalosis accompanying respiratory acidosis often involves hyponatremia, hypokalemia, and hypochloremia, which should be corrected as needed. Metabolic alkalosis caused by hypokalemia and hypochloremia is often iatrogenic and should be prevented.
Arrhythmias
These commonly present as atrial premature beats and paroxysmal supraventricular tachycardia, with chaotic atrial tachycardia being the most characteristic. Atrial flutter and atrial fibrillation may also occur. Most arrhythmias resolve after infection control and correction of hypoxemia, acid-base, and electrolyte imbalances. Persistent arrhythmias may require specific medications.
Shock
Although rare, shock indicates a poor prognosis when it occurs. Causes include severe infections, hemorrhage (often due to upper gastrointestinal hemorrhage), and severe heart failure or arrhythmias.
Gastrointestinal Hemorrhage
Chronic cor pulmonale may lead to gastrointestinal hemorrhage due to infection, respiratory failure, heart failure, gastrointestinal congestion, or corticosteroid use. Preventive measures and active management are necessary when hemorrhage occurs.
Disseminated Intravascular Coagulation (DIC)
This is discussed in DIC.
Deep Vein Thrombosis (DVT)
Low-dose unfractionated heparin or low-molecular-weight heparin can be used for prevention.
Prognosis
Chronic cor pulmonale often involves recurrent acute exacerbations, with progressive worsening as pulmonary function declines. The prognosis is generally poor, with a mortality rate of approximately 10-15%. However, active treatment can prolong survival and improve the quality of life.
Prevention
Prevention focuses on managing and treating underlying bronchial, pulmonary, and pulmonary vascular diseases. Efforts should aim to prevent the development and progression of pulmonary hypertension and chronic cor pulmonale.