Acute respiratory distress syndrome (ARDS) is acute respiratory failure caused by various pulmonary and extrapulmonary pathogenic factors. The main pathological feature of ARDS is acute lung injury due to inflammatory responses, characterized by damage to the pulmonary microvascular endothelium and alveolar epithelium, increased microvascular permeability, and exudation of protein-rich fluid into the alveolar space, leading to pulmonary edema, hyaline membrane formation, and extensive alveolar collapse. The primary pathophysiological changes include reduced lung volume, decreased lung compliance, and severe ventilation-perfusion mismatch characterized by shunt. Clinically, it presents with respiratory distress and refractory hypoxemia, with bilateral infiltrative changes on lung imaging.
Etiology
The causes of ARDS are numerous and can be divided into pulmonary (direct) and extrapulmonary (indirect) factors. However, these direct and indirect factors, along with the resulting inflammatory responses, imaging changes, and pathophysiological reactions, often overlap. In recent years, social development and medical advancements have changed the distribution of ARDS causes. E-cigarette-associated lung injury has emerged as a new cause of ARDS in young adults. Advances in cancer treatment have made chemotherapy drugs and immune checkpoint inhibitors important causes of drug-induced ARDS. Additionally, viral infections have long been a major cause of ARDS.
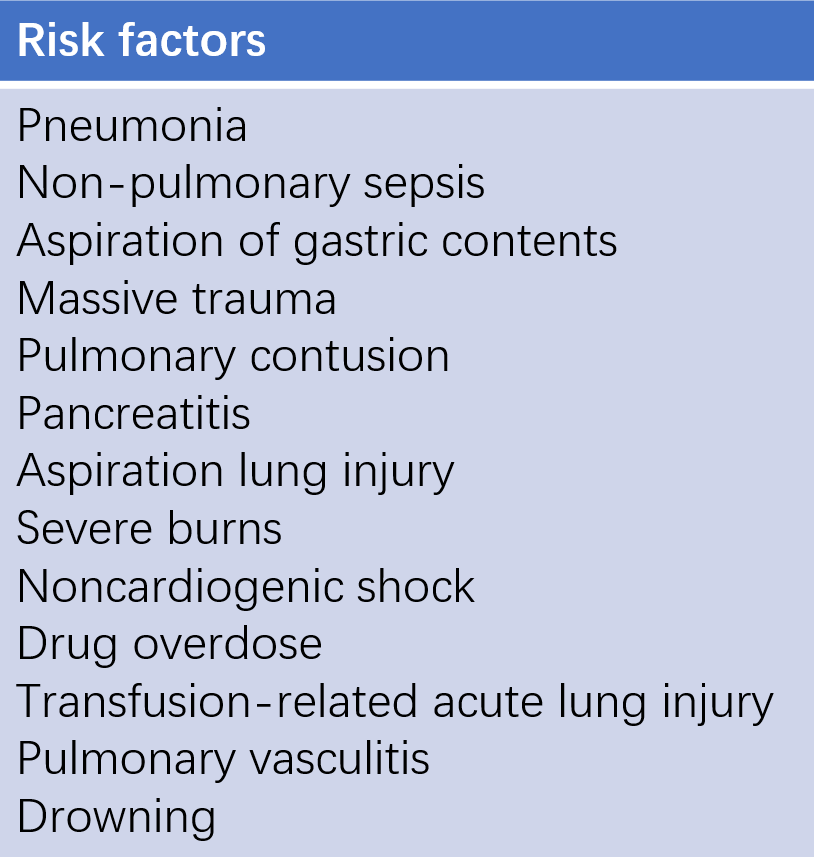
Table 1 Risk factors for ARDS
Pathology and Pathophysiology
The pathological process of ARDS can be roughly divided into three overlapping phases: exudative phase, proliferative phase, and fibrotic phase.
Exudative Phase
The first 7 days after ARDS onset are pathologically known as exudative phase, and are characterized by diffuse alveolar damage (DAD), including damage to pulmonary capillary endothelial cells and alveolar epithelial cells. Type I alveolar epithelial cells are damaged and necrotic, with protein-rich edema fluid and inflammatory cell infiltration in the interstitium and alveolar spaces. Pulmonary microvasculature presents with congestion, hemorrhage, and microthrombi formation. After about 72 hours, a hyaline membrane forms from coagulated plasma proteins, cell debris, fibrin, and residual pulmonary surfactant, accompanied by focal or extensive alveolar collapse. The lungs are dark red or dark purple, hepatized, with significantly increased weight, edema, hemorrhage, and fluid exudation from the cut surface, which is termed wet lung. Increased alveolar membrane permeability and decreased surfactant lead to interstitial and alveolar edema, small airway closure, and alveolar collapse.
CT reveals inhomogeneous distribution of pulmonary edema and atelectasis, predominantly in dependent regions (posterior lung areas in supine position) with poor ventilation, normal alveolar ventilation in the non-dependent regions (anterior chest wall areas in supine position), and reduced functional residual capacity and effective alveolar gas exchange, leading to the description of ARDS lung as baby lung or small lung. These changes result in decreased lung compliance, increased intrapulmonary shunt, refractory hypoxemia, and respiratory distress.
The mechanisms of respiratory distress include:
- Hypoxemia stimulates carotid and aortic body chemoreceptors, reflexively stimulating the respiratory center, causing hyperventilation
- Pulmonary congestion and edema stimulate J receptors, reflexively deepening and accelerating breathing, leading to respiratory distress
Initial PaCO2 may be reduced or normal due to respiratory compensation. Increased pulmonary vascular resistance due to microvascular occlusion and reduced functional residual capacity can lead to pulmonary hypertension, increased dead space, and acute cor pulmonale and hypercapnia in severe patients.
Proliferative Phase
The phase is generally 7 - 21 days after ARDS onset. Some patients experience further lung injury and early fibrosis. The typical histological changes are the resorption and resolution of inflammatory exudates and hyaline membranes, with alveolar exudates organizing and lymphocytic infiltration replacing neutrophils. As part of the repair process, type II alveolar epithelial cells proliferate along the alveolar basement membrane, synthesizing and secreting new surfactant and differentiating into type I alveolar epithelial cells.
Fibrotic Phase
Although the lung function recovers in most ARDS patients 3 - 4 weeks after onset, ARDS in some patients progresses to the fibrotic phase, potentially requiring long-term mechanical ventilation and (or) oxygen therapy. Histologically, early alveolar inflammatory edema transforms into alveolar and interstitial fibrosis. Significant destruction of acinar structure leads to emphysema-like changes and bullae formation. These pathological changes decrease lung compliance and reexpandability, increasing the risk of barotrauma. The reduction in pulmonary microvascular bed, thickened alveolar septa, intimal fibrosis of pulmonary microvessels, and microthrombi cause vascular occlusion, increasing dead space, leading to gas exchange impairment and refractory hypercapnia. Increased pulmonary microcirculation resistance raises pulmonary circulation pressure, resulting in pulmonary hypertension.
Clinical Manifestations
ARDS typically occurs within 72 hours after the onset of the primary disease, rarely exceeding 7 days. In addition to the symptoms and signs of the primary disease, the earliest symptoms are tachypnea, progressively exacerbated dyspnea, and cyanosis, often accompanied by restlessness, anxiety, and perspiration. The dyspnea is characterized by deep, rapid, and labored respiration, and patients often feel chest tightness and severe breathlessness, which is termed respiratory distress, and cannot be alleviated by standard oxygen therapy and cannot be explained by other primary cardiopulmonary conditions such as pneumothorax, emphysema, atelectasis, pneumonia, and heart failure. Early signs may be unremarkable or may include fine moist crackles in both lungs. In the late stage, examination often reveals coarse crackles and possibly bronchial breath sounds.
Auxiliary Examination
Chest X-ray and CT
Early x-ray may show no abnormalities or mild interstitial changes, with increased lung markings and hazy edges. This progresses to bilateral patchy or confluent ground-glass opacities or consolidation. The changes are consistent with pulmonary edema, showing rapid variability. Chest x-ray in the late stage may show pulmonary interstitial fibrosis. Although CT is more accurate than x-ray, its high radiation and the high risk of transporting critically ill patients limit its widespread use. Currently, ARDS diagnosis primarily relies on chest x-ray.
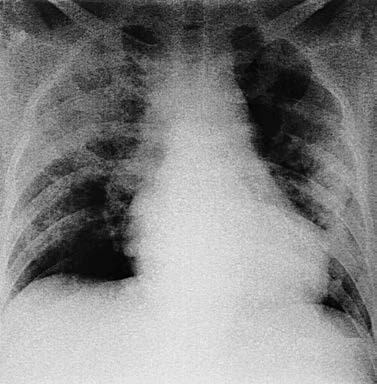
Figure 1 Extensive patchy infiltration in both lungs on the chest x-ray
Pulmonary Ultrasound
Bilateral multiple B-lines and (or) consolidation are indicative of ARDS on pulmonary ultrasound. Ultrasound is convenient, safe, and allows dynamic assessment. It is sensitive but has moderate specificity and interoperator variability, which may increase false positives. Therefore, evaluations should be performed by trained ultrasound professionals.
Arterial Blood Gas Analysis
Typical changes include decreased PaO2, decreased PaCO2, and increased pH. Oxygenation indices, such as the oxygenation index (PaO2/FiO2), alveolar-arterial oxygen gradient [P(A-a)O2], and intrapulmonary shunt (QS/QT), are important for diagnosis, severity grading, and treatment evaluation. PaO2/FiO2 is most common in clinical practice, with normal values of 400 - 500 mmHg. In the early stage, respiratory alkalosis may occur due to hyperventilation, with pH above normal and PaCO2 below normal. In the late stage, if dead space ventilation increases, respiratory muscles fatigue, or metabolic acidosis occurs, pH may fall below normal and PaCO2 may rise above normal.
SpO2/FiO2
When SpO2 ≤ 97%, SpO2/FiO2 correlates well with PaO2/FiO2. Therefore, when arterial blood gas analysis is unavailable, SpO2/FiO2 can substitute for PaO2/FiO2 to assess oxygenation and ARDS severity.
Bedside Respiratory Function Monitoring
In ARDS, pulmonary edema, decreased lung compliance, and significant intrapulmonary shunt occur, without airflow limitation. Bedside respiratory mechanics monitoring often indicates low compliance, relatively normal resistance, and high shunt rates. These changes are significant for assessing ARDS severity and treatment efficacy.
Cardiac Ultrasound and Swan-Ganz Catheterization
Cardiac ultrasound helps differentiate cardiogenic pulmonary edema and guide treatment, offering non-invasive, radiation-free, and repeatable advantages. If conditions allow, cardiac ultrasound should be routinely performed when diagnosing ARDS. Swan-Ganz catheter measurement of pulmonary artery wedge pressure (PAWP) > 18 mmHg suggests acute left heart failure and cardiogenic pulmonary edema, but ARDS and cardiogenic pulmonary edema can coexist. Thus, PAWP > 18 mmHg is not an exclusion criterion for ARDS. If respiratory failure cannot be fully explained by left heart failure, ARDS should still be considered. Due to high risk and complications, Swan-Ganz catheterization is no longer a routine method for differentiating cardiogenic pulmonary edema.
Diagnosis
Diagnostic criteria include:
- Induction by various acute factors such as pneumonia, extrapulmonary infections, trauma, aspiration, shock, and transfusion
- Acute respiratory failure or respiratory failure exacerbation occurring within 1 week under clear precipitating factors
- Exclusion of pulmonary edema primarily due to cardiac origin/fluid overload and hypoxemia mainly caused by atelectasis
- Chest x-ray or CT showing bilateral infiltrates, or chest ultrasound (by trained professionals) indicating bilateral B-lines or consolidation
- Oxygenation indices
Oxygenation Indices
In non-intubated patients:
- HFNC flow ≥ 30 L/min or expiratory positive airway pressure (EPAP) or continuous positive airway pressure (CPAP) ≥ 5 cm H2O in noninvasive positive pressure ventilation (NPPV), PaO2/FiO2 ≤ 300 mmHg or SpO2/FiO2 ≤315 mmHg (and SpO2 ≤97%)
In intubated patients:
- Mild ARDS: 200 mmHg < PaO2/FiO2 ≤300 mmHg or 235 mmHg < SpO2/FiO2 ≤315 mmHg (and SpO2 ≤97%)
- Moderate ARDS: 100 mmHg < PaO2/FiO2 ≤200 mmHg or 148 mmHg < SpO2/FiO2 ≤235 mmHg (and SpO2 ≤97%)
- Severe ARDS: PaO2/FiO2 ≤100 mmHg or SpO2/FiO2 ≤148 mmHg (and SpO2 ≤97%)
In resource-limited settings:
- ARDS diagnosed based solely on SpO2/FiO2 ≤315 mmHg (and SpO2 ≤97%) without the requirement of PEEP or HFNC flow
Differential Diagnosis
The above ARDS diagnostic criteria are nonspecific. Since ARDS is a clinical syndrome with various causes, identifying the etiology is crucial. When establishing a diagnosis, it is essential to exclude cardiogenic pulmonary edema, large atelectasis, massive pleural effusion, and diffuse alveolar hemorrhage. Identification can usually be achieved through detailed medical history, physical examination, chest x-ray, cardiac ultrasound, and blood tests. In cardiogenic pulmonary edema, dyspnea is exacerbated in supine position, pink frothy sputum is present, and lung crackles are more prominent at the lung bases, responding well to inotropes and diuretics. If differentiation is difficult, echocardiography to assess ventricular function can aid in diagnosis and guide treatment.
Treatment
The treatment principles include treatment of the primary disease, support of organ function, and management of complications.
Treatment of the Primary Disease
This is the primary principle and foundation for treating ARDS. It is crucial to actively identify and adequately treat the triggers of ARDS. Infection is the most common trigger, and ARDS can also lead to secondary infections. Therefore, infection should be suspected in all ARDS patients unless there is a clear alternative cause. Antibiotic selection should be empirical and based on the immune status, site of infection, severity, and risk of multidrug-resistant organisms.
Correction of Hypoxia
The goal for oxygen therapy in ARDS patients is a PaO2 of 55 - 80 mmHg or an SaO2 of 88% - 95%. The minimum oxygen concentration that achieves the target should be used, and the method of oxygen therapy should be chosen based on the severity of hypoxemia.
Mechanical Ventilation
Although there are no unified criteria for mechanical ventilation in ARDS, it is mostly recommended mechanical ventilation should be initiated once ARDS is diagnosed. Mild ARDS patients may attempt noninvasive positive pressure ventilation (NPPV) under close monitoring. If high-concentration oxygen or NPPV fails to improve hypoxemia or if significant respiratory distress occurs, invasive mechanical ventilation should be initiated early. The goal is to maintain adequate ventilation and oxygenation to support organ function. Due to the heterogeneous and small lung characteristics of ARDS, the key is to recruit collapsed alveoli and keep them open, increasing lung volume and improving oxygenation while avoiding alveolar overdistension and repetitive opening and closing injuries. A lung-protective ventilation strategy is recommended, including low tidal volume ventilation, higher positive end-expiratory pressure (PEEP), and prone positioning in severe ARDS patients.
Low Tidal Volume Ventilation
This involves using low tidal volumes and limiting plateau pressure. It is strongly recommended a tidal volume of 4 - 8 ml/kg of ideal body weight, with inspiratory plateau pressure kept below 30 cm H2O should be used to prevent alveolar overdistension. Some patients may experience CO2 retention and respiratory acidosis (pH > 7.2) when using protective ventilation strategies. Accepting hypercapnia and continuing the ventilation strategy is known as permissive hypercapnia, where the presence of hypercapnia is tolerated rather than corrected.
PEEP Adjustment
Appropriate PEEP levels can open collapsed airways and alveoli, increase end-expiratory lung volume, reduce lung injury and alveolar edema, and improve alveolar diffusion function and ventilation-perfusion ratio, reducing intrapulmonary shunt, thereby improving oxygenation and lung compliance. It also prevents shear injury from alveolar collapse and reopening. Higher PEEP levels are recommended for moderate to severe ARDS patients. However, PEEP can increase intrathoracic pressure, reduce venous return, and potentially exacerbate lung injury. The optimal PEEP determination is still under debate and can be guided by tools such as optimal oxygenation methods, esophageal pressure monitoring, and electrical impedance tomography (EIT).
Prone Positioning
Prone positioning improves oxygenation by reducing thoracic pressure gradients, redistributing lung fluids, and promoting secretion drainage, thereby reducing mortality in severe ARDS patients. It is strongly recommended for at least 12 hours daily in severe ARDS patients. During the procedure, close monitoring of endotracheal tubes and intravascular catheters is necessary. Contraindications include severe hypotension, ventricular arrhythmias, increased intracranial pressure, facial trauma, and unstable spinal fractures.
Lung Recruitment
Low tidal volume ventilation to limit airway plateau pressure may not favor the recruitment of collapsed alveoli in ARDS, and the effect of PEEP in keeping alveoli open depends on the degree of alveolar inflation during inspiration. Therefore, transiently increasing airway pressure can reopen collapsed alveoli, reducing intrapulmonary shunt and improving oxygenation.
Neuromuscular Blockers
Excessive respiratory drive in ARDS patients increases oxygen consumption and the risk of barotrauma. Neuromuscular blockers relax skeletal muscles, improve patient-ventilator synchrony, and reduce oxygen consumption. However, long-term use increases the risk of ICU-acquired weakness and ventilator-associated pneumonia. Short-term use (no more than 48 hours) is recommended in early severe ARDS patients with refractory hypoxemia, patient-ventilator asynchrony, barotrauma risk, and requirement for prone positioning.
Extracorporeal Membrane Oxygenation (ECMO)
ECMO provides temporary support for refractory respiratory and (or) circulatory failure patients. Current clinical research results on ECMO are inconsistent. ECMO may be considered as a salvage treatment for severe ARDS patients with reversible primary disease. Specific indications include mechanical ventilation duration < 7 days, severe hypoxemia and (or) respiratory acidosis despite lung-protective ventilation in combination with prone positioning, neuromuscular blockers, lung recruitment measures, and optimized ventilator settings (FiO2 ≥ 0.8, tidal volume of 6 ml/kg in ideal body weight, PEEP ≥ 10 cm H2O): PaO2/FiO2 < 50 mmHg for >3 hours, or PaO2/FiO2 < 80 mmHg for >6 hours; pH < 7.25 with PaCO2 ≥ 60 mmHg for >6 hours when respiratory rate is increased to 35 breaths/min with adjusted ventilator settings to keep plateau pressure ≤ 32 cm H2O,. ECMO can be considered if there are no contraindications to anticoagulation.
Fluid Management
The inflammatory response in ARDS increases capillary permeability and causes pulmonary edema. Compared to a liberal fluid management strategy, a restrictive fluid management approach, ensuring organ perfusion based on central venous pressure and urine output monitoring, can improve oxygenation, and shorten mechanical ventilation time, but does not reduce mortality.
Glucocorticoids
Due to their potent anti-inflammatory effects, glucocorticoids have been a focus of ARDS treatment research.
Anticoagulation Therapy
ARDS patients are in a hypercoagulable state due to severe hypoxia, systemic inflammatory response, and immobilization, increasing the risk of deep vein thrombosis and pulmonary embolism. Thrombosis and hemorrhage risks should be assessed, and prophylactic anticoagulation should be provided if there are no contraindications.
Nutritional Support
ARDS patients are in a hypermetabolic state and require adequate nutritional support. In hemodynamically stable ARDS patients, enteral nutrition should be initiated early (within 24-48 hours after ICU admission) if there are no contraindications. If enteral nutrition cannot be initiated, parenteral nutrition can be temporarily provided, transitioning to enteral nutrition as soon as possible. In patients in prone positioning, post-pyloric feeding is preferred to reduce the risk of reflux and aspiration.
Prevention of Ventilator-associated Pneumonia (VAP)
VAP is the most common complication in ARDS patients. In mechanically ventilated patients, bundled preventive measures should be implemented to avoid VAP.
Early Rehabilitation
Early rehabilitation in ARDS patients can reduce the incidence of ICU-acquired weakness, shorten mechanical ventilation duration, and decrease mortality.
Prognosis
The mortality rate of ARDS is 26% - 44%. Prognosis is significantly related to the primary disease and severity. Patients with pneumonia secondary to sepsis or immunocompromised individuals with opportunistic infections have a poor prognosis. Only 16% of ARDS patients die solely from respiratory failure; 49% die from multiple organ dysfunction syndrome (MODS). Older patients (over 60 years) have a poor prognosis. In recent years, ARDS mortality has shown a declining trend. Most survivors recover full lung function, while some patients have residual pulmonary fibrosis.