In adults, a sinus rhythm with a frequency exceeding 100 beats per minute is termed sinus tachycardia. Clinically, it is categorized into physiological sinus tachycardia and inappropriate sinus tachycardia.
Physiological sinus tachycardia is commonly seen in healthy individuals during smoking, drinking tea or coffee, alcohol consumption, physical activity, and emotional excitement. It can also occur in certain pathological states such as fever, hyperthyroidism, anemia, shock, myocardial ischemia, heart failure, and the use of medications such as adrenaline and atropine.
Inappropriate sinus tachycardia is characterized by a persistent increase in heart rate at rest, or a heart rate increase that is unrelated or disproportionate to physiological, emotional, pathological states, or medication effects. Its mechanism is unclear but may be related to increased automaticity of the sinoatrial node or abnormal autonomic regulation of the sinoatrial node.
Sinus tachycardia usually begins and ends gradually, with a frequency typically between 100 and 150 beats per minute. Treatment should target the etiology and remove precipitating factors, such as treating heart failure, correcting anemia, and controlling hyperthyroidism. If necessary, β-blockers or non-dihydropyridine calcium channel blockers such as diltiazem can be used alone or in combination. If these medications are ineffective or not tolerated, the If current inhibitor ivabradine may be considered.
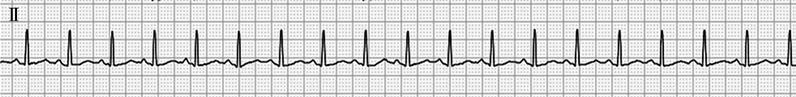
Figure 1 Sinus tachycardia
In lead II, the P wave is positive, the PR interval is 0.13 seconds, and the heart rate is 115 beats per minute.