Under normal physiological conditions, adenoids grow rapidly in children between the ages of 2 and 6 years and begin to gradually atrophy after the age of 10, eventually disappearing in adulthood. Significant pathological enlargement of adenoids during childhood that leads to a series of clinical symptoms is referred to as adenoid hypertrophy.
Etiology
Adenoid hypertrophy is often caused by recurrent adenoid infections or by inflammation from nearby regions, such as the nasal cavity, sinuses, or tonsils, extending to the nasopharynx and stimulating pathological hyperplasia of the adenoids.
Clinical Manifestations
Local Symptoms
Adenoid hypertrophy affects multiple areas, including the ears, nose, throat, and larynx.
Ear Symptoms
Obstruction of the pharyngeal opening of the Eustachian tube may lead to secretory otitis media, resulting in hearing loss and tinnitus, and in some cases, purulent otitis media may occur.
Nasal Symptoms
Conditions such as rhinitis and sinusitis often develop concurrently, leading to nasal congestion and excessive nasal discharge. Speech may exhibit a nasal tone, and during sleep, snoring and mouth breathing are common. Severe cases may result in obstructive sleep apnea (OSA).
Symptoms of the Pharynx, Larynx, and Lower Respiratory Tract
Secretions irritate the respiratory mucosa, often causing paroxysmal coughing and increasing susceptibility to tracheitis.
Impact of Chronic Mouth Breathing on Craniofacial Development
Prolonged mouth breathing affects facial growth, resulting in elongation of the maxilla, retrusion of the mandible, a high-arched palate, dental malocclusion, prominence of the upper incisors, thickened lips, and a lack of facial expression, collectively referred to as “adenoid face.”
Systemic Symptoms
These primarily include chronic intoxication and reflexive neurological symptoms, such as developmental delays, sluggish responses, poor concentration, night terrors, teeth grinding, and enuresis.
Examinations
Adenoid face may be observed during visual inspection in some patients. Examination of the oropharynx may reveal purulent secretions attached to the posterior wall of the pharynx, a high and narrow hard palate, and frequently enlarged palatine tonsils. Fiberoptic (or electronic) nasopharyngoscopy shows hypertrophic adenoids obstructing the posterior nasal choanae. Lateral X-rays of the nasopharynx assess adenoid size and the degree of airway obstruction. Polysomnography may reveal varying degrees of sleep apnea or hypopnea. CT and MRI scans of the nasopharynx may help measure adenoid size and differentiate it from other conditions, such as rhinosinusitis or nasopharyngeal tumors.
Adenoid hypertrophy is classified into four grades based on the degree of obstruction of the posterior nasal choanae observed with fiberoptic (or electronic) nasopharyngoscopy:
- Grade I: Obstruction ≤ 25%
- Grade II: Obstruction 26%–50%
- Grade III: Obstruction 51%–75%
- Grade IV: Obstruction > 75%
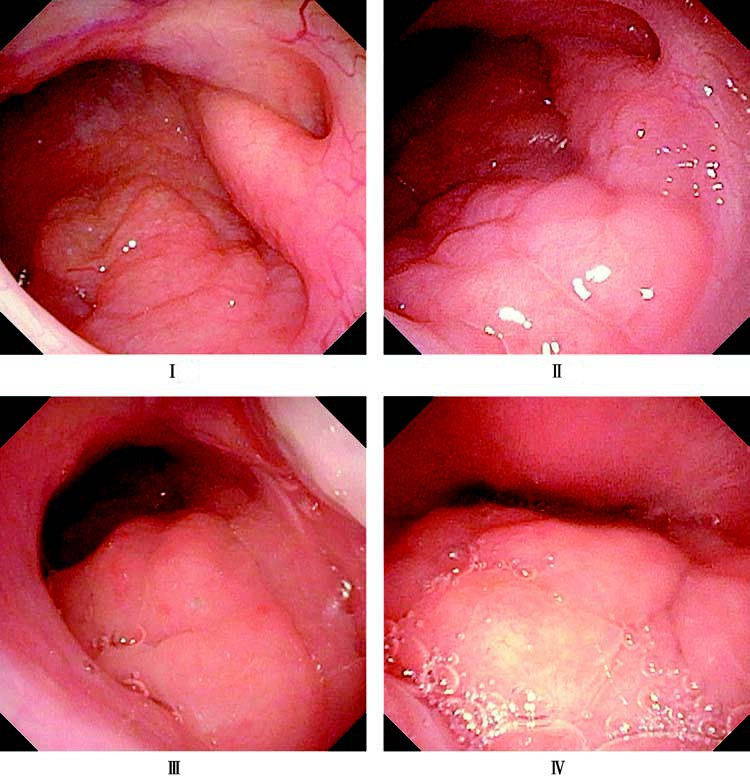
Figure 1 Grading of adenoid hypertrophy
Treatment
General Management
Improved nutrition, prevention of infections, and strengthening the body's immunity are central principles of management. Attention to underlying conditions is essential. Symptoms may alleviate or resolve completely as the child grows older and the adenoids gradually atrophy.
Surgical Treatment
Indications for adenoidectomy include:
- Airway obstruction, especially in pediatric OSA cases.
- Concurrent secretory otitis media unresponsive to conservative treatment, which may require both tympanostomy tube placement and adenoidectomy.
- Persistent or recurrent sinusitis as part of a stepwise treatment strategy.
- Chronic mouth breathing as a causal factor in maxillary protrusion, treated through adenoidectomy as part of the therapeutic plan.
Preoperative evaluations should carefully rule out contraindications, such as acute infectious diseases or bleeding disorders. If indications exist for simultaneous palatine tonsillectomy, both procedures may be performed together.