Sinus pause or sinus arrest is the failure of the sinoatrial node to generate impulses. Electrocardiogram shows an interval significantly longer than the normal PP interval without the occurrence of a P wave, or the absence of both P waves and QRS complexes. The prolonged PP interval does not have a multiplicative relationship with the basic sinus PP interval. After a prolonged sinus pause, lower potential pacemakers, such as the atrioventricular junction or ventricles, may emit a single escape beat or an escape rhythm to control the ventricles.
Sinus arrest is commonly seen in conditions such as sinoatrial node degeneration and fibrosis, acute inferior myocardial infarction, cerebrovascular accidents, increased vagal tone, or carotid sinus hypersensitivity. Additionally, the use of digitalis glycosides, acetylcholine, and similar agents can also cause sinus arrest. If a sinus pause lasts too long (more than 3 seconds) without an escape beat, patients may experience symptoms such as amaurosis fugax, transient loss of consciousness, and syncope. In severe cases, Adams-Stokes syndrome or even death may occur. Treatment can be seen in sick sinus syndrome.
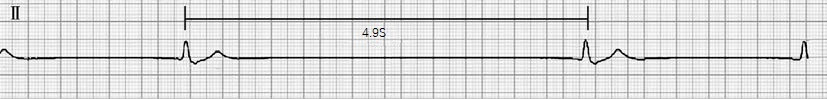
Figure 1 Sinus arrest with ventricular escape beat
In lead II, there is no sinus P wave, the longest RR interval is 4.9 seconds, and the QRS complexes are wide and abnormal, with a duration of 0.12 seconds.