Sinoatrial block (SAB) is the delay or blockage of impulse conduction from the sinoatrial node to the atria. Theoretically, SAB can be classified into three degrees. However, since body surface electrocardiogram cannot display sinoatrial node electrical activity, it is not possible to diagnose first-degree and third-degree SAB using a body surface ECG.
Second-degree SAB is divided into two types:
- Mobitz type I (Wenckebach block), characterized by progressively shorter PP intervals until a long PP interval occurs, which is shorter than twice the basic PP interval.
- Mobitz type II, where the long PP interval is a multiple of the basic PP interval.
After sinoatrial block, an escape rhythm may occur. The etiology and treatment of sinoatrial block can be seen in sick sinus syndrome.
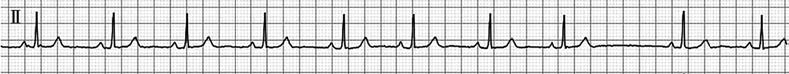
Figure 1 Second-degree type I sinoatrial block
In lead II, the sinus PP interval gradually shortens until a long PP interval appears. The long PP interval (1.47 seconds) is shorter than twice the basic PP interval (0.95 seconds).