Olfactory neuroblastoma, also known as esthesioneuroblastoma, is a malignant tumor originating from the olfactory epithelium and accounts for 3%–5% of all nasal malignancies. The annual incidence rate is approximately 0.04 per 100,000 individuals and is more common in females. The age of onset demonstrates a bimodal distribution, with the most common occurrences at 2 years of age and 60 years of age.
Etiology
Olfactory neuroblastoma is a malignant tumor derived from the neuroectoderm, although its exact etiology remains unclear. It may arise due to malignant transformation of residual embryonic cells.
Pathology
Macroscopically, olfactory neuroblastomas often appear as unilateral polypoid masses with a glossy, soft, gray-red appearance and are highly vascularized, making them friable and prone to bleeding.
Under a light microscope, tumor cells are submucosal and exhibit well-circumscribed nests, lobules, or sheets. The stroma is edematous, and the tumor nests are surrounded by vascular-rich fibrous stroma, giving a characteristic lobular pattern. These structural features are diagnostic. However, early undifferentiated tumors may lack clear distinguishing features in light microscopy, making it difficult to differentiate them from other small-round-cell sinonasal tumors.
Clinical Manifestations
The clinical presentation of olfactory neuroblastoma is closely related to the tumor's growth. Common sites of occurrence include the nasal roof, the posterior-superior part of the nasal septum, the cribriform plate, and the superior nasal concha. The tumor often extends to the cranial base and intracranial region. It usually presents as a polypoid lesion, though some cases may appear nodular. The tumor is friable and easily bleeds.
In the early stages, symptoms may be absent. As the disease progresses, unilateral nasal obstruction, epistaxis, and headache may gradually develop, resembling nasal inflammatory symptoms. Local extension into the orbit can result in diplopia, tearing, proptosis, and even blindness. Intracranial involvement may lead to anosmia and cranial nerve palsies. In advanced stages, regional lymph node metastasis and distant metastases may occur.

Figure 1 Endoscopic appearance of olfactory neuroblastoma
Imaging Studies
Tumors in infants and young children are often located in the anterior nasal cavity, while in adults, they are typically found in the middle and posterior nasal cavity. Imaging studies reveal both expansive and infiltrative bone destruction. Tumors frequently invade the ethmoid sinuses unilaterally or bilaterally. Superior extension may involve the cribriform plate and, along the olfactory nerves, infiltrate the anterior cranial fossa and brain parenchyma, forming intracranial and extracranial contiguity. Radiologically, this presents as a "doughnut-like" or "mushroom-like" lesion centered on the cribriform plate. Laterally, the tumor may destroy the lateral orbital wall (paper-thin lamina) and invade the orbit. It can also extend posteriorly through the superior orbital fissure to involve the optic nerve.

Figure 2 CT imaging of olfactory neuroblastoma (coronal view)
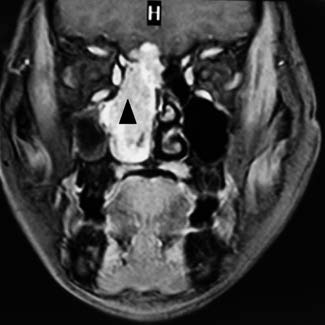
Figure 3 MR imaging of olfactory neuroblastoma (coronal view)
Diagnosis
Pathological biopsy remains the gold standard for diagnosing olfactory neuroblastoma. The diagnosis is based on histopathological features and immunohistochemical markers. If cervical lymph node metastasis is suspected, fine-needle aspiration and biopsy can confirm the diagnosis. Whole-body imaging techniques such as CT, MRI, and PET scans are essential for detecting distant metastases and planning further treatment strategies.
Treatment
The primary treatment modalities for olfactory neuroblastoma include surgery, radiotherapy, and chemotherapy.
Surgical Treatment
Surgical intervention offers the advantage of achieving substantial or radical tumor resection. Aside from alleviating compression symptoms caused by the tumor, surgery also allows for better evaluation of tumor staging and histology, while preserving brain tissue and nerve function to the extent possible. However, given the local invasiveness of olfactory neuroblastoma and difficulty in defining clear surgical margins, recurrence and metastasis may occur even after treatment, which can negatively impact prognosis. Therefore, long-term surveillance is essential after surgery. A combination of surgery with adjuvant radiotherapy and chemotherapy based on histopathological findings offers improved disease-free survival rates.
Radiotherapy
Radiotherapy is primarily used for locally advanced tumors as neoadjuvant therapy, as well as for palliative care in metastatic cases. Stereotactic radiotherapy plays a crucial role in the treatment of small local recurrences. However, long-term neurotoxicity due to radiotherapy may affect prognosis and requires careful consideration.
Chemotherapy
Chemotherapy is particularly effective for olfactory neuroblastoma and shows good efficacy, especially in cases of locally advanced or metastatic disease.
Currently, a multidisciplinary treatment strategy centered on surgery is recommended to improve patient survival outcomes and quality of life.