Facial nerve tumors are rare, usually benign, and slow-growing neoplasms. They can occur at any segment of the facial nerve, from the cerebellopontine angle to the facial region, with the geniculate ganglion and adjacent segments being the most commonly affected sites. These tumors primarily affect middle-aged individuals, without differences in incidence between sexes or sides.
Based on pathological characteristics, facial nerve tumors can be classified into facial nerve schwannoma, facial nerve neurofibroma, and facial nerve hemangioma. Among these, schwannomas are more common, neurofibromas are less frequent, while hemangiomas are rare. The underlying mechanisms of these tumors remain unclear, though they are suspected to be associated with genetic mutations. Facial nerve schwannomas originate from Schwann cells that surround facial nerve fibers and are also referred to as facial nerve Schwann cell tumors.
Clinical Manifestations
Facial Paralysis
Gradual or fluctuating weakness of the facial muscles may occur. In early stages, there may be no symptoms or signs, but progressive peripheral facial paralysis develops over time.
Abnormal Facial Movement and Sensation
Patients may experience facial spasms, pain, or numbness.
Hearing Loss and Tinnitus
Conductive hearing loss may occur due to tumor effects on or disruption of the ossicular chain and tympanic membrane. When the tumor involves the labyrinthine segment, the internal auditory canal segment, or compresses the cochlear nerve, it can lead to sensorineural hearing loss. Some patients may also present with pulsatile tinnitus.
Vertigo
Tumors affecting the vestibular system, semicircular canals, or internal auditory canal can cause varying degrees of vertigo.
Other Associated Symptoms
Dry eyes, taste disturbances, and hyperacusis may occur. Tumors involving the intracranial segment and compressing nearby cranial nerves can result in corresponding symptoms.
External Auditory Canal Narrowing
In addition to peripheral facial paralysis, some patients show posterior wall protrusion of the external auditory canal, leading to narrowing or obstruction of the canal.
Parotid Mass
When the facial nerve tumor is located within the parotid gland or affects multiple segments of the facial nerve involving the parotid region, it may present as a mass within the parotid gland.
Auxiliary Examinations
Imaging Studies
High-Resolution Temporal Bone CT
This can reveal localized destruction of the facial nerve canal along its course, with expansile soft tissue masses or irregular focal lesions. Tumors confined to the geniculate ganglion or labyrinthine segments may show enlargement in the "T-shaped" area. Those at the geniculate ganglion may extend into the middle cranial fossa.
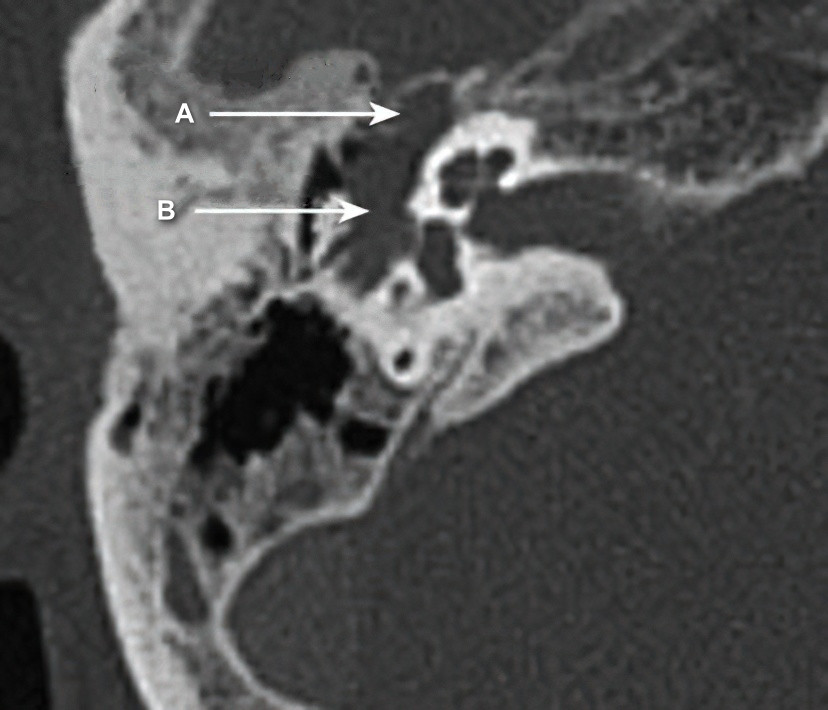
Figure 1 CT scan shows a space-occupying lesion involving the right geniculate ganglion and horizontal segment of the facial nerve, accompanied by right middle ear effusion.
A: Space-occupying lesion in the geniculate ganglion
B: Space-occupying lesion in the tympanic segment of the facial nerve

Figure 2 CT reconstruction reveals a space-occupying lesion in the horizontal and vertical segments of the left facial nerve.
A: Facial nerve canal reconstruction shows enlargement due to a space-occupying lesion in the facial nerve canal
Enhanced Temporal Bone MRI
Tumors show isointense signals on T1-weighted images, similar to those of soft tissues, and appear as isointense or hyperintense on T2-weighted images. Tumors with high water content display high signal intensity on T2-weighted images, while those with low water content appear isointense. Lesion signals are usually inhomogeneous. Larger tumors may show cystic changes due to liquefaction necrosis. Contrast-enhanced MRI demonstrates intense or mixed enhancement. Typical facial nerve schwannomas exhibit oval-shaped lesions, while neurofibromas often present as elongated cord-like lesions.
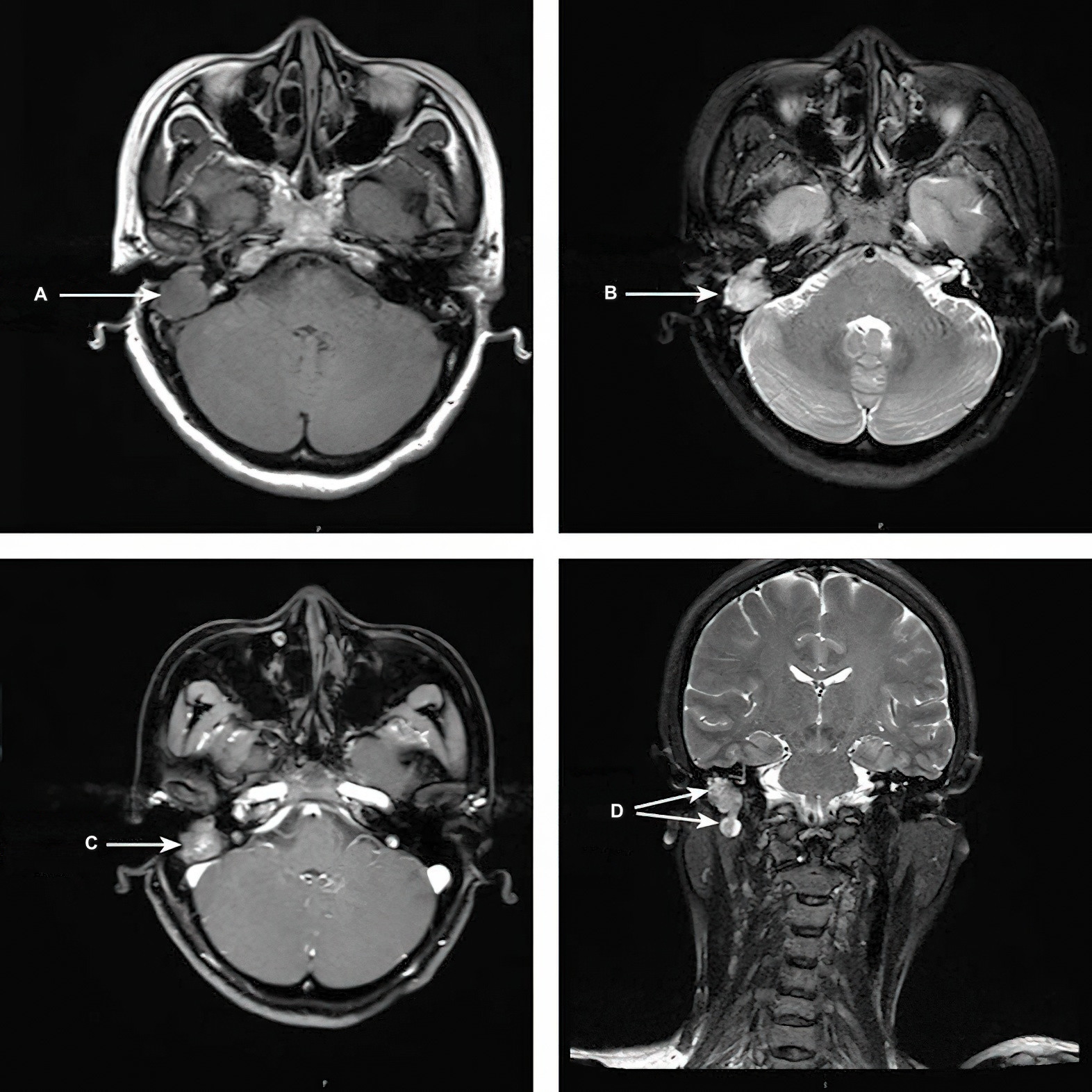
Figure 3 MRI with contrast enhancement demonstrates a space-occupying lesion in the vertical segment of the right facial nerve.
A, B, C: Space-occupying lesion in the vertical segment of the facial nerve
D: Lobulated space-occupying lesion in the vertical segment of the facial nerve
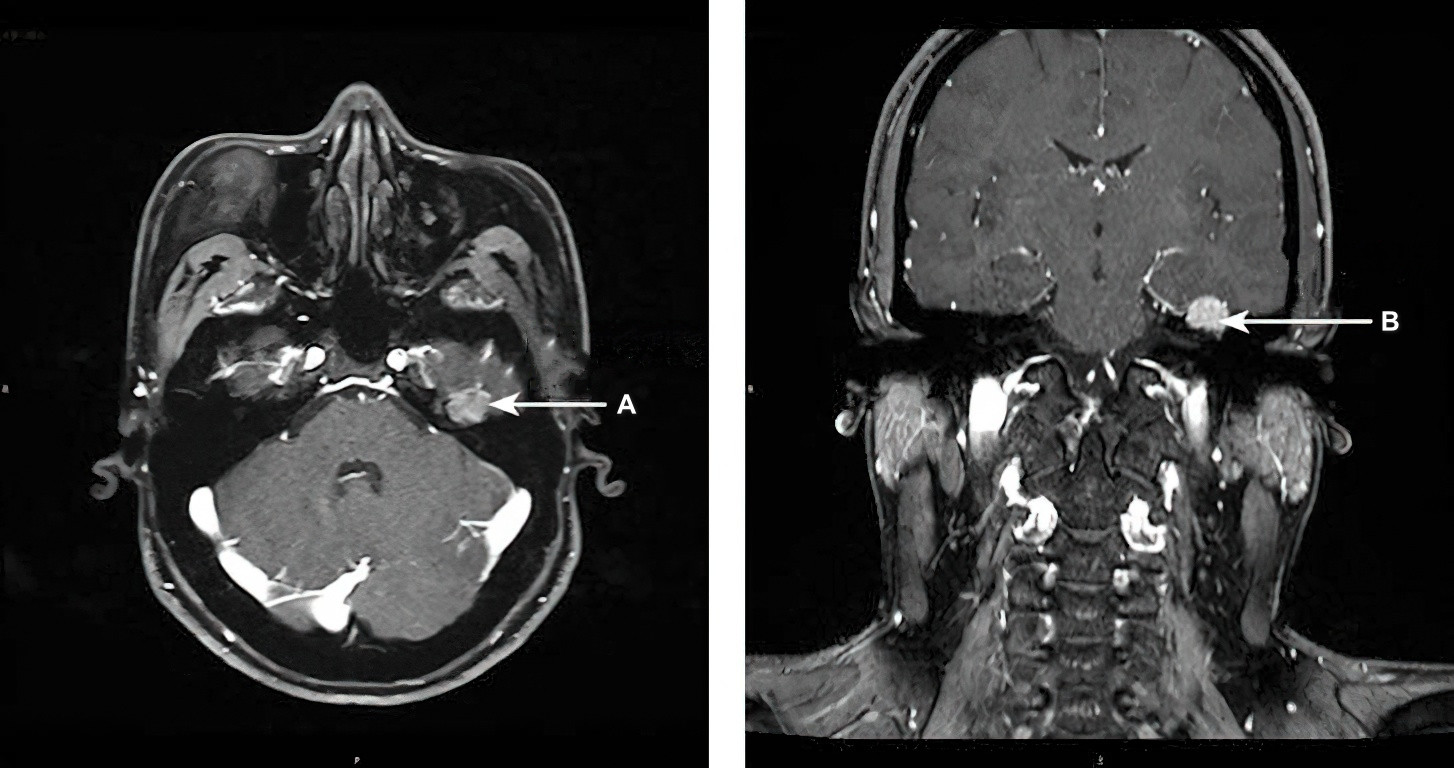
Figure 4 MRI with contrast enhancement (T1-weighted imaging) indicates a space-occupying lesion in the left geniculate ganglion.
A, B: Space-occupying lesion in the geniculate ganglion
Facial Nerve Function Tests
Neural Excitability Test (NET)
A lack of response to a 10mA stimulus indicates loss of innervation, while a stimulus threshold difference greater than 3.5mA between the two sides suggests irreversible facial nerve impairment.
Electromyography (EMG) and Electroneurography (EnoG)
Absence of myoelectrical activity indicates complete facial nerve paralysis. The degree of degeneration is assessed by comparing the amplitude ratio of the affected and unaffected sides, which indicates varying degrees of facial nerve degeneration, up to complete degeneration.
Diagnosis
The diagnosis is often straightforward based on the patient's medical history, clinical manifestations, and imaging findings. Confirmation, however, may require intraoperative exploration and histopathological examination of the lesion.
Differential Diagnosis
Vestibular Schwannoma
Facial nerve tumors occurring at the cerebellopontine angle and internal auditory canal need to be distinguished from vestibular schwannomas. Vestibular schwannomas rarely cause facial paralysis, whereas facial nerve tumors in these locations often involve the labyrinthine segment, demonstrated by enlargement and destruction of the labyrinthine portion.
Bell’s Palsy
Facial nerve tumors in the temporal bone segment require differentiation from Bell’s palsy. Imaging studies aid in excluding or confirming the presence of space-occupying lesions, as Bell’s palsy does not present with lesions on imaging.
Jugular Paraganglioma
Facial nerve tumors involving the jugular foramen region need to be differentiated from jugular paragangliomas, which show the characteristic "salt-and-pepper" enhancement pattern on MRI.
Other Parotid Gland Tumors
When facial nerve tumors occur in the extratemporal segment, they need to be differentiated from other parotid gland tumors. Benign parotid tumors generally do not cause facial paralysis, while malignant tumors often feel firm on palpation, lack clear boundaries, and exhibit ill-defined margins on imaging. In contrast, facial nerve tumors in the extratemporal segment typically present as well-defined lesions on imaging.
Middle Ear Carcinoma and Other Malignant Tumors
When symptoms such as ear pain, blood-tinged discharge, and bone destruction not following the course of the facial nerve are present, middle ear carcinoma and other malignant tumors should be excluded.
Treatment
During tumor resection, preserving the integrity of the facial nerve trunk is often not feasible. The tumor and the affected portion of the facial nerve are typically resected together, followed by procedures to restore facial nerve function. Facial nerve grafting or reconstruction using techniques such as facial nerve–hypoglossal nerve anastomosis usually results in House-Brackmann (H-B) grades III–IV, with significant synkinesis, making complete recovery of normal facial nerve function challenging. For patients with normal or only mild facial paralysis, controversy exists regarding the necessity and timing of surgery. Surgical intervention is generally recommended when irreversible H-B grade III or higher facial nerve dysfunction or intracranial compression symptoms occur.
Observation and Regular Follow-Up
For patients with small, asymptomatic tumors, observation and periodic monitoring through follow-up are appropriate.
Surgical Treatment
Based on tumor size, various approaches such as the transmastoid approach, trans-tympanic and supralabyrinthine approaches, translabyrinthine approach, middle cranial fossa approach, or a combined mastoid–middle cranial fossa approach can be selected for tumor excision. The tumor and the affected segment of the facial nerve should be resected together, with visualization of the normal facial nerve stumps at both ends. Facial nerve functionality can be restored using techniques like facial nerve grafting, facial nerve–hypoglossal nerve anastomosis, or facial nerve–masseteric nerve anastomosis.