Acoustic neuroma (AN), first documented in the literature in 1777, is a benign tumor originating from the eighth cranial nerve. Since the tumor predominantly arises from the Schwann cells of the vestibular nerve sheath, it is also referred to as vestibular schwannoma (VS). The incidence of AN is approximately 10–13 per 1,000,000 individuals, accounting for about 6%–10% of intracranial tumors and 80%–90% of cerebellopontine angle (CPA) tumors. This tumor is more commonly observed in adults, with a peak incidence between 30 and 50 years of age, and there are no significant differences across races or genders. Most cases involve unilateral tumors, while bilateral acoustic neuromas are frequently associated with neurofibromatosis type II.
Etiology and Pathology
AN most commonly originates from the vestibular nerve sheath within the internal auditory canal, with the inferior vestibular nerve being the most frequent source, followed by the superior vestibular nerve. Tumors arising from the cochlear nerve are rare. The tumor typically appears gray-red, pale yellow, or gray-white in color and may be spherical, oval, or doughnut-like, with smooth and regular surfaces and abundant vascularization. The tumor is enclosed in a thin layer of connective tissue but lacks a complete capsule. Internally, its structure is highly heterogeneous, with textures ranging from soft to hard, and some areas may exhibit cystic degeneration. The tumor generally grows slowly, with significant individual variability, with reports suggesting an average annual growth of 0.4–2.4 mm.
Based on the cellular arrangement, AN can be classified into two types:
- Antoni A type: Dense fibrous arrangement, with spindle cells forming parallel, whorled, or palisade-like patterns.
- Antoni B type: Sparse reticular arrangement, with loosely arranged reticular cells in a palisade-like pattern.
Both Antoni A and Antoni B patterns may be observed within the same tumor.
Clinical Manifestations
Clinical symptoms are directly related to the tumor's location and size. Tumors confined to the internal auditory canal primarily present with hearing loss, tinnitus, and vestibular dysfunction. With extension into the CPA, hearing loss may worsen, cerebellar compression may cause balance disorders, and trigeminal nerve compression may lead to ipsilateral facial numbness or neuralgia. Further tumor growth may compress the brainstem, resulting in hydrocephalus, headaches, nausea, and vomiting.
Unilateral progressive hearing loss is the most common early symptom of AN, although some patients may present with sudden hearing decline in the affected ear.
Unilateral tinnitus is also common, usually presenting as persistent high-pitched tinnitus, and it may occur before hearing loss becomes apparent.
Vestibular dysfunction typically manifests as mild dizziness or unsteady gait, which may resolve over days to weeks. Larger tumors may compress the cerebellum, leading to impaired coordination, unsteady gait, and leaning toward the affected side.
In addition to the vestibulocochlear nerve, the trigeminal nerve is the most commonly affected, with symptoms such as a foreign body sensation in the cornea, facial numbness, pain, or sensory disturbances. Compression of the posterior cranial nerve group (cranial nerves IX–XI) is less common.
Headaches are often described initially as stabbing or dull pain in the occipital region. When hydrocephalus and intracranial hypertension develop, symptoms may progress to severe headaches, nausea, and vomiting. In severe cases, brain herniation may lead to death.
Auxiliary Examinations
Comprehensive audiologic, vestibular function, and imaging examinations are required for suspected cases of acoustic neuroma.
Audiological Testing
Pure tone audiometry typically shows sensorineural hearing loss, with high-frequency hearing being most affected. The hearing loss may show either a gradual decline or a steep drop-off pattern. Approximately 1% of patients in the early stage of the disease may have normal hearing. Speech recognition testing may show markedly reduced speech discrimination relative to the degree of hearing loss, with noticeable declines even when pure-tone thresholds show only mild impairment.
Auditory brainstem response (ABR) is currently the most sensitive audiologic test for acoustic neuroma. Prolongation of wave V latency is a hallmark finding, with interaural latency differences of wave V often exceeding 0.4 ms. However, 10%–15% of patients may have completely normal ABR results.
Vestibular Function Testing
Abnormal findings on electronystagmography are observed in 70%–90% of patients with acoustic neuroma. During caloric testing, reduced or absent responses on the affected side are typical findings.
Imaging Studies
Imaging examinations include high-resolution CT of the temporal bone and enhanced MRI. The positivity rate of high-resolution CT is 60%–70%. CT typically reveals iso- or hypodense CPA mass lesions, often without calcification. Bone window CT may display widened and eroded internal auditory canals, with inhomogeneous enhancement after contrast administration. However, small tumors within the internal auditory canal (less than 5 mm) may be missed.
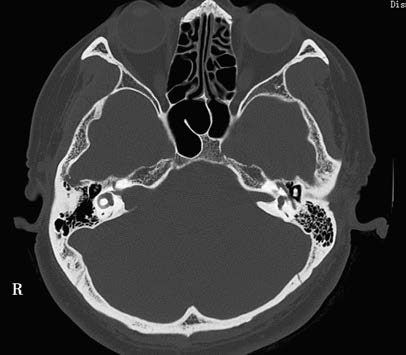
Figure 1 CT findings of acoustic neuroma in the temporal bone
The right internal auditory canal is enlarged, displaying a funnel-shaped appearance.
MRI is the most sensitive and effective method for diagnosing acoustic neuroma. Contrast-enhanced MRI can detect tumors as small as 1 mm in the internal auditory canal. Typical imaging characteristics include:
- T1-weighted images showing mildly hypointense or isointense signals, while T2-weighted images show hyperintense signals.
- The tumor appearing as a round or semicircular mass with an apex pointing toward the fundus of the internal auditory canal, resembling the "ice cream cone" sign.
- The tumor showing homogeneous, inhomogeneous, or annular enhancement following intravenous contrast injection, depending on the proportion and distribution of solid and cystic components within the tumor.

Figure 2 MRI findings of acoustic neuroma
A space-occupying lesion is observed in the right internal auditory canal and cerebellopontine angle. On T1-weighted imaging (T1WI), the lesion exhibits hypointense signals, while on T2-weighted imaging (T2WI), it appears hyperintense. The tumor shows significant enhancement, with portions exhibiting cystic degeneration.
Differential Diagnosis
It is essential to differentiate acoustic neuroma from conditions such as meningioma, facial nerve schwannoma, schwannomas of the trigeminal nerve and posterior cranial nerves, cerebellopontine angle epidermoid cysts, arachnoid cysts, gliomas, as well as inner ear diseases such as sudden hearing loss and Ménière's disease.
Treatment
Treatment Strategy
The treatment plan for acoustic neuroma involves comprehensive considerations, including the size and location of the tumor, preoperative hearing and balance function, as well as the patient's age and overall health. There are three main treatment options:
Microsurgery
Complete surgical removal remains the primary treatment option. Surgery is recommended for patients with significant tumor growth, substantial hearing loss, vertigo, or large tumors causing compressive symptoms such as headache and ataxia. Surgery is also considered when radiotherapy fails to control tumor growth.
Imaging-Based Observation
Observation is suitable for small tumors confined to the internal auditory canal with minimal or no growth and preserved hearing, or for asymptomatic elderly patients (70 years and older). Periodic MRI assessments are required, with the second imaging examination conducted six months after the initial diagnosis, followed by annual imaging thereafter. If the tumor shows significant growth or clinical symptoms worsen, surgical intervention or stereotactic radiotherapy may be considered.
Stereotactic Radiotherapy
This approach is primarily reserved for patients who are older, have systemic health issues that contraindicate surgery, or have non-cystic tumors smaller than 3 cm in diameter that show persistent growth or worsening symptoms. It may also be an option for patients who refuse surgery. However, it should be noted that stereotactic radiotherapy can only control tumor growth, and in cases where surgery is required later, it may reduce the preservation rate of facial and other cranial nerve functions.
Surgical Goals
With continuous advancements in surgical and monitoring techniques, the goals of acoustic neuroma surgery have evolved from simply reducing mortality to preserving facial and auditory nerve function. The ideal acoustic neuroma surgery aims to achieve the following:
- Complete tumor resection.
- High facial nerve function preservation rate.
- Preservation of hearing in patients with functional preoperative hearing.
Additionally, the prevention of severe neurological complications is a critical consideration.
Surgical Approaches
The selection of a surgical approach depends on factors such as tumor size, preoperative hearing status, the patient’s age and overall health, as well as the surgeon's expertise. The primary surgical approaches include the translabyrinthine approach, middle cranial fossa approach, and retrosigmoid approach. The translabyrinthine and middle cranial fossa approaches are classic surgical techniques initially developed by otologic surgeons.