Cardiovascular implantable electronic devices (CIEDs) include pacemakers (PMs), implantable cardioverter-defibrillators (ICDs), and cardiac resynchronization therapy (CRT) devices. Initially used for treating bradyarrhythmias, these devices have expanded to manage tachyarrhythmias and heart failure, with ICDs and CRTs playing significant roles. The rapid advancements in device implantation technology have greatly improved patient quality of life and reduced major adverse cardiovascular events. Additionally, the advanced storage and diagnostic capabilities of pacemakers aid in arrhythmia diagnosis and cardiac electrophysiology study.
Pacemakers are mainly used to treat bradycardia, while ICDs are primarily for converting ventricular tachycardia and defibrillating ventricular fibrillation. CRT devices treat chronic heart failure by resynchronizing the contraction of the left and right ventricles through pacing pulses.
Pacemaker Therapy
Pacemakers deliver electrical impulses to stimulate the heart, mimicking normal cardiac impulse formation and conduction, to treat various types of bradyarrhythmias. With technological advances, pacemakers have become smaller yet more powerful.
A pacemaker consists of electrode leads and a pulse generator. The leads are implanted through veins into the appropriate heart chambers, and the pacemaker is placed in a subcutaneous pocket. Recently, leadless pacemakers, which integrate the pulse generator and electrode into a single unit, have been introduced. These are implanted directly into the heart chamber as a miniaturized capsule, eliminating the need for transvenous leads and subcutaneous pockets, making them suitable for patients with abnormal conventional pacing pathways or recurrent systemic infections. Temporary pacing is a short-term solution for critical arrhythmias, mainly used in symptomatic or hemodynamically unstable bradycardia, and can also suppress tachyarrhythmias. Temporary pacemakers are often used as emergency measures, typically for no more than two weeks.
Indications
Indications include:
- Symptomatic sinus node dysfunction
- Symptomatic chronic bifascicular or trifascicular block, and second-degree type II, high-degree, or third-degree atrioventricular block; persistent atrial fibrillation with symptomatic bradycardia
- Symptomatic sinus node dysfunction or atrioventricular block caused by arrhythmias or other diseases requiring medication (without alternative treatment options)
- Cardioinhibitory carotid sinus syndrome or syncope due to cardiac arrest (>3 seconds) during tilt-table testing
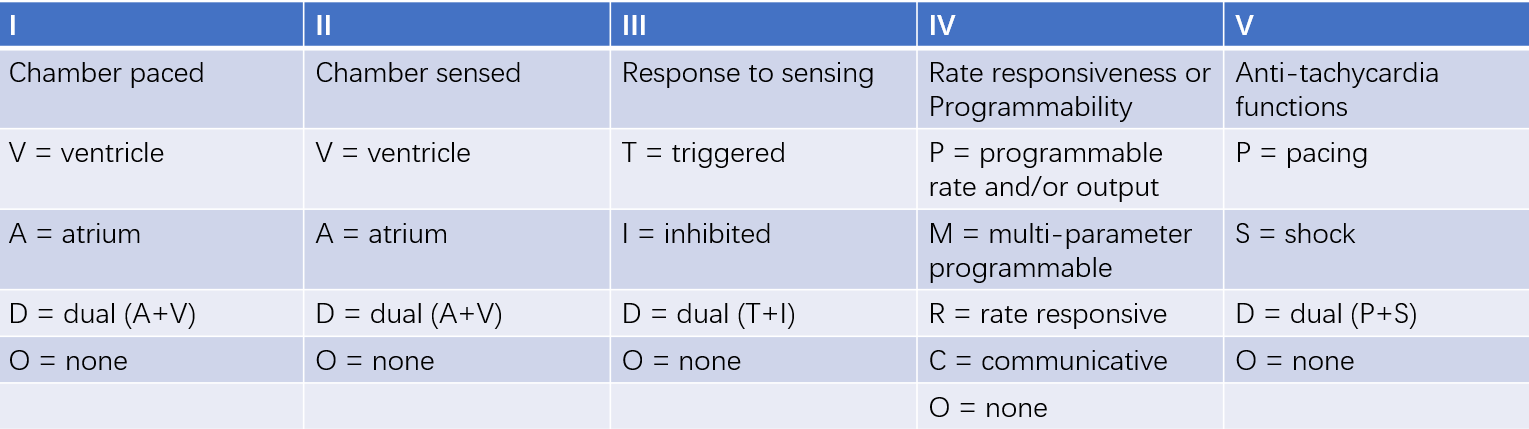
Table 1 NBG codes
Pacemaker Functions and Modes
As the types and modes of pacemakers increase, their functions become more complex. To facilitate communication among doctors, technicians, and patients, NBG code was introduced.
Understanding and remembering the meanings of pacemaker codes is crucial. For example, the VVI pacing mode indicates that the pacemaker paces the ventricle, senses intrinsic ventricular signals, and inhibits a pacing pulse when an intrinsic signal is detected. The DDD pacing mode paces both the atrium and ventricle, senses signals from both, and can inhibit or trigger a pulse during the refractory period. The AAIR mode paces the atrium, senses atrial signals, inhibits pacing upon detection, and adjusts pacing rate based on patient needs, which is known as rate-responsive pacing (indicated by the fourth letter R). Other pacing modes include VDD and DDI.
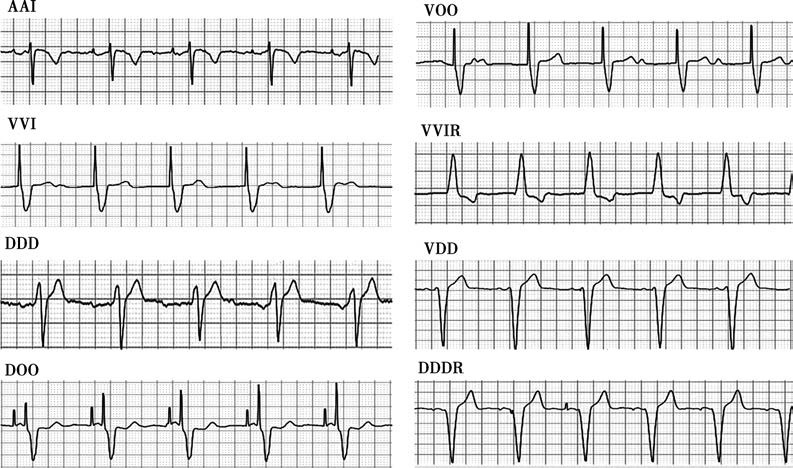
Figure 1 Schematic diagram of different pacing modes
Clinical Classification based on Electrode Lead Placement
Single-chamber pacemakers include VVI pacemakers (with leads typically placed in the right ventricular apex, septum, His bundle, or left bundle branch area) and AAI pacemakers (with leads usually placed in the right atrial appendage or low atrial septum). These pacemakers provide timely pacing to the ventricle or atrium based on rate needs.
Dual-chamber pacemakers have two leads placed in the right atrial appendage or low atrial septum (atrium) and the right ventricular apex, septum, His bundle, or left bundle branch area (ventricle), enabling atrioventricular sequential pacing.
Selection of Pacing Modes
VVI Mode is suitable for all types of bradyarrhythmias, but is not recommended if:
- Blood pressure drops by more than 20 mmHg during VVI pacing
- Poor cardiac function compensation
- Patients with pacemaker syndrome, where VVI pacing disrupts atrioventricular sequential contraction, leading to symptoms due to reduced cardiac output
AAI mode maintains atrioventricular sequential contraction, and is considered physiological pacing, suitable for sick sinus syndrome with normal atrioventricular conduction, but is not recommended if:
- Atrioventricular conduction block, including potential risk (tested with atrial pacing)
- Chronic atrial arrhythmias
DDD mode is the most comprehensive in dual-chamber pacemakers, pacing and sensing both atrium and ventricle, and is suitable for atrioventricular block with or without sinus node dysfunction. It is not recommended for patients with chronic atrial fibrillation or flutter.
Rate-responsive (R) mode adjusts pacing rate based on sensing physical activity and blood pH to meet cardiac output needs and improve exercise tolerance. It is suitable for those engaging in moderate to heavy physical activity, with options like VVIR, AAIR, and DDDR. It is not recommended for patients whose symptoms worsen with increased heart rate or who develop heart failure or angina.
In summary, the principles for selecting the best pacing mode are:
- For sinus node dysfunction with normal atrioventricular conduction, AAI mode is best.
- For complete atrioventricular block with normal sinus node function, VDD mode is optimal.
- For dysfunction in both sinus node and atrioventricular conduction, DDD mode is preferred.
- For those needing moderate to heavy physical activity, rate-responsive pacing can be used.
Implantable Cardioverter-Defibrillators
ICDs are multifunctional electronic devices with programmable parameters that terminate life-threatening arrhythmias. They are implanted with endocardial defibrillation electrodes to sense ventricular tachycardia and fibrillation and deliver anti-tachycardia pacing or defibrillation energy to terminate tachyarrhythmias. The first ICD was used in 1980 on a survivor of sudden cardiac death (SCD). Today, ICDs are among the most effective means of preventing SCD.
ICDs provide anti-bradycardia pacing, anti-tachycardia pacing (ATP), low-energy cardioversion, and high-energy defibrillation. Recently, subcutaneous ICDs (S-ICDs) have been used clinically, but since their electrodes and pulse generator are subcutaneous, they lack anti-bradycardia and anti-tachycardia pacing functions.
Indications
ICD indications include:
- Survivors of hemodynamically unstable sustained ventricular tachycardia (VT) or ventricular fibrillation (VF) due to irreversible causes
- Patients with irreversible VF or hemodynamically unstable VT occurring 48 hours after myocardial infarction; and those with left ventricular ejection fraction (LVEF) ≤35% and NYHA class II-III, or LVEF ≤30% and NYHA class I, 40 days after myocardial infarction and 90 days after revascularization, after optimized medical therapy
- Patients with non-ischemic cardiomyopathy with LVEF ≤35% and NYHA class II-III after 3 - 6 months of optimized medical therapy
- Patients with unexplained syncope where electrophysiological testing induces sustained VT or VF with significant hemodynamic changes
- Patients with hypertrophic cardiomyopathy, dilated cardiomyopathy, or arrhythmogenic right ventricular cardiomyopathy at risk of sudden cardiac death
- Patients with inherited heart diseases, such as long QT syndrome or Brugada syndrome, who have syncope or recorded VT and are unresponsive to β-blockers
Cardiac Resynchronization Therapy
CRT is an implantable electronic device that adds left ventricular pacing to conventional right atrial and right ventricular dual-chamber pacing. By setting appropriate atrioventricular and interventricular pacing intervals, it corrects dyssynchrony in contraction, improving cardiac efficiency and increasing cardiac output. CRT in combination with ICD is known as CRT-D. CRT has become a crucial treatment for heart failure patients with reduced ejection fraction and wide QRS complexes, further reducing mortality.
Indications
CRT indications include:
- Patients with heart failure symptoms despite optimized medical therapy, complete left bundle branch block (LBBB) (QRS duration > 130 ms), LVEF ≤ 35%, and NYHA class II-III
- Patients with heart failure symptoms despite optimized medical therapy, incomplete LBBB (QRS duration ≥ 150 ms), LVEF ≤ 35%, and NYHA class II-III
- Patients with indications for ventricular pacing or high-degree atrioventricular block and LVEF < 40%
- Patients with persistent atrial fibrillation and LVEF < 40% with poor ventricular rate control who are candidates for atrioventricular node ablation
Follow-up
The main purpose of pacemaker follow-up is to monitor patient condition, evaluate device status, track disease progression, and facilitate communication. The details include assessing device performance, optimizing parameter settings, identifying and correcting system issues, predicting battery life, determining replacement timing, maintaining records of patient and device programming changes, and providing patient education and support. For ICD patients, appropriate programming of tachycardia detection and therapy parameters is advised to reduce ICD shocks. Psychological assessment and intervention are recommended for patients with inappropriate or frequent ICD discharges to alleviate anxiety and improve quality of life. For CRT patients, optimizing resynchronization parameters is crucial to ensure a high percentage of resynchronized pacing and enhance CRT response. Follow-up plans should be individualized based on clinical conditions, reviewing heart failure diagnostic parameters (transthoracic impedance, nighttime heart rate, heart rate variability, patient activity) to adjust treatment plans for maximum benefit.
Follow-up includes clinic visits and remote monitoring. All cardiovascular implantable electronic devices require in-office follow-up in the early period (1 - 3 months after implantation); mid-term follow-up is recommended every 6 - 12 months either in clinic or via remote monitoring; late-term follow-up (approaching battery end of life) is recommended every 1 - 3 months in clinic or via remote monitoring.