Stable angina pectoris, also known as exertional angina pectoris, is characterized by paroxysmal squeezing chest pain or chest tightness, primarily located behind the sternum. The pain may radiate to the precordial area and the ulnar side of the left upper limb. It typically occurs during increased physical exertion, lasts for a few minutes, and subsides with rest or after taking nitrate medications. The severity, frequency, duration, nature of the pain, and triggering factors remain relatively unchanged over several months.
Pathogenesis
When coronary arteries are narrowed or partially obstructed, blood flow to the myocardium is reduced, and oxygen supply becomes relatively fixed. At rest, the balance between myocardial oxygen supply and demand can be maintained, and the patient may remain asymptomatic. However, during exertion, emotional stress, overeating, or exposure to cold, the sudden increase in cardiac workload leads to elevated heart rate, myocardial tension, and contractility, resulting in increased myocardial oxygen consumption. If the narrowed coronary arteries cannot provide sufficient blood flow to meet the myocardial oxygen demands, angina occurs.
Pathological Anatomy and Pathophysiology
Coronary angiography in patients with stable angina shows that approximately 25% have significant stenosis (≥70% narrowing) in one, two, or three coronary arteries. About 5-10% have significant stenosis in the left main coronary artery. In the remaining 15% of patients, no significant coronary artery stenosis is observed, suggesting that coronary artery spasm, microvascular dysfunction, excessive sympathetic activity, excessive catecholamine secretion, or abnormal myocardial metabolism may contribute to insufficient myocardial blood and oxygen supply.
Before an angina attack, patients often exhibit elevated blood pressure, increased heart rate, and elevated pulmonary artery pressure and pulmonary capillary wedge pressure, reflecting reduced compliance of the heart and lungs. During an attack, left ventricular systolic function may be impaired, with reduced contractility, slower ejection velocity, decreased left ventricular systolic pressure, reduced stroke volume and cardiac output, and increased left ventricular end-diastolic pressure and volume. These changes indicate both systolic and diastolic dysfunction of the left ventricle. The left ventricular wall may show asynchrony in contraction or localized hypokinesia.
Clinical Manifestations
Symptoms
The primary clinical manifestation of angina is episodic chest pain.
Triggers
Common triggers include physical exertion or emotional stress (e.g., anger, anxiety, or overexcitement). Other triggers include overeating, cold exposure, smoking, tachycardia, and shock. Pain typically occurs during exertion or emotional stress rather than after exertion. Typical stable angina recurs under similar conditions.
Location
The pain is primarily located behind the sternum and may extend to the precordial area, covering an area roughly the size of a palm. It may also radiate across the anterior chest, with poorly defined boundaries. Pain often radiates to the left shoulder, the inner side of the left arm (reaching the ring and little fingers), or to the neck, throat, or jaw.
Nature
The chest pain is often described as oppressive, constrictive, or tight, and may sometimes feel like a burning sensation. However, it is not typically sharp or stabbing. In rare cases, it may be accompanied by a sense of impending doom. Some patients experience only chest tightness or discomfort, or dyspnea, rather than chest pain. During an attack, patients are often forced to stop their activities until symptoms subside.
Duration
The pain usually lasts a few minutes to more than ten minutes, most commonly 3-5 minutes, and rarely exceeds 30 minutes.
Relief
The symptoms typically resolve after stopping the activity that triggered the attack. Sublingual or inhaled nitrate medications, such as nitroglycerin, can also relieve symptoms within minutes.
Signs
No abnormal physical signs are typically present between episodes. During an angina attack, the following signs may be observed:
- Increased heart rate
- Elevated blood pressure
- Anxious facial expression
- Cold or sweaty skin
- Occasionally, a gallop rhythm (third or fourth heart sound)
Transient systolic murmurs at the apex may occur during an attack, caused by mitral regurgitation secondary to ischemic dysfunction of the papillary muscles.
Auxiliary Examinations
Laboratory Tests
Blood glucose and lipid levels can be used to assess risk factors for coronary artery disease (CAD). In cases of significant chest pain, tests for cardiac troponin I or T, creatine kinase (CK), and its isoenzyme CK-MB are performed to differentiate stable angina from acute coronary syndrome (ACS). N-terminal pro-B-type natriuretic peptide (NT-proBNP) is used to evaluate cardiac function. Complete blood count (CBC) is used to check for anemia. Thyroid function tests can be performed when necessary.
Electrocardiogram (ECG)
Resting ECG
Approximately half of patients show normal resting ECG results. Some may exhibit changes indicative of previous myocardial infarction or nonspecific ST-segment and T-wave abnormalities. Occasionally, arrhythmias such as atrioventricular or bundle branch block, atrial or ventricular premature beats may be observed, but these findings are nonspecific.
ECG During Angina Attack
Most patients show transient ST-segment changes due to myocardial ischemia. Subendocardial ischemia, which is more common, typically manifests as ST-segment depression (≥0.1 mV). These changes resolve after the episode subsides. T-wave inversion may also occur. In patients with persistent T-wave inversion at baseline, the T-wave may become upright during an attack (pseudonormalization). Although T-wave changes are less specific for myocardial ischemia compared to ST-segment depression, significant differences from baseline ECG can aid in diagnosis.
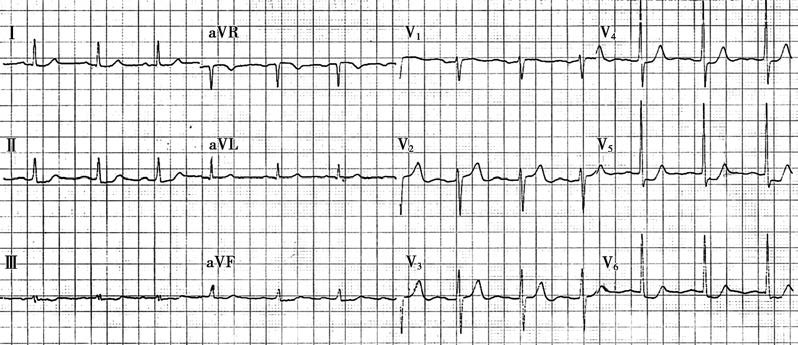
Figure 1 Electrocardiogram (ECG) during angina attack
Leads I, II, III, aVF, and V4-V6 show ST-segment depression.
Exercise Stress Test
The most used stress test involves exercise to provoke myocardial ischemia by increasing cardiac workload. Graded treadmill or bicycle ergometry is typically used, with exercise intensity gradually increased. The patient performs exercise until reaching the age-predicted maximum heart rate (HRmax) or a submaximal target heart rate (85-90% of HRmax). ECG changes are monitored continuously during exercise. ECG recordings are taken at baseline, during each stage of exercise, immediately after stopping, and every 2 minutes thereafter until heart rate returns to baseline. Blood pressure is measured simultaneously with ECG recordings. A positive stress test is indicated by the occurrence of typical angina and/or ST-segment depression (horizontal or downsloping ≥0.1 mV, 60-80 ms after the J-point) lasting for at least 2 minutes.
The test should be terminated immediately if the patient develops angina, gait instability, ventricular tachycardia, or a drop in blood pressure. Contraindications for exercise stress testing include acute myocardial infarction, unstable angina, significant heart failure, severe arrhythmias, and acute illnesses.
The test has a certain rate of false positives and false negatives, so results alone cannot confirm or rule out CAD.
Holter Monitoring
Holter monitoring continuously records and automatically analyzes ECG over 24 hours (or longer) using bipolar chest leads or synchronized 12-lead ECG. It can detect ST-segment and T-wave changes (ST-T abnormalities) and various arrhythmias. Correlating abnormal ECG findings with patient activity and symptoms can help diagnose angina. Ischemic ST-T changes corresponding to the time of chest pain episodes support the diagnosis of angina and can also detect silent myocardial ischemia.
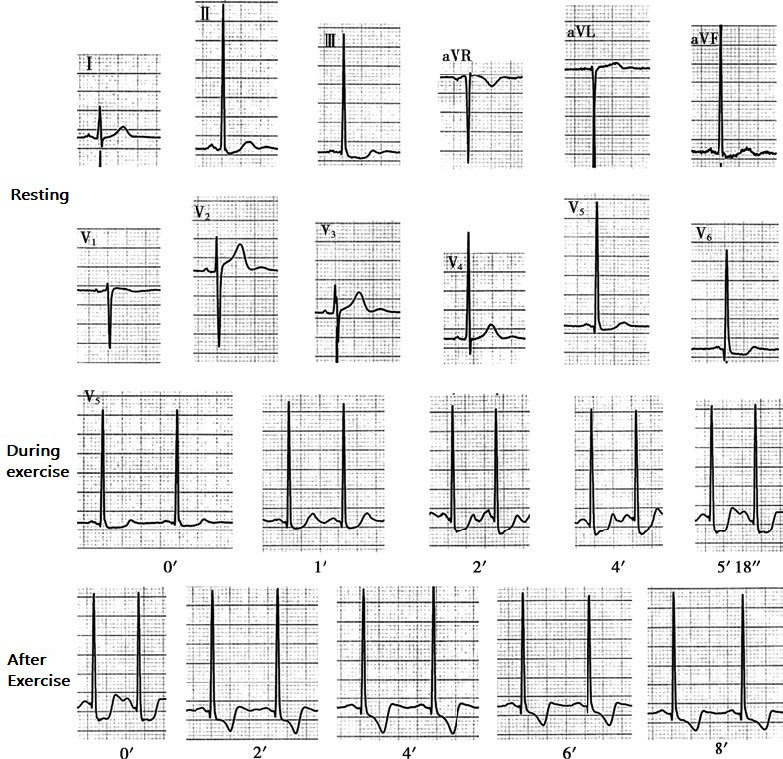
Figure 2 ECG treadmill stress test
At rest, the ECG shows ST-segment depression in leads II, III, aVF, V5, and V6. During exercise, ST-segment depression begins in lead V5 at 1 minute and reaches 4 mm at 5 minutes and 18 seconds. After exercise, ST-segment depression and T-wave inversion are observed in leads I, II, III, aVF, V3, V4, V5, and V6, and these changes persist for 8 minutes without recovery. The stress test result is positive.
CT Angiography (CTA)
CTA allows for two-dimensional or three-dimensional reconstruction of coronary arteries. It is used to assess the degree of coronary artery stenosis and the extent of arterial wall calcification. CTA can also provide information on the distribution and characteristics of plaques within the arterial wall. CTA has a high negative predictive value. If no significant stenosis is observed, invasive testing is generally unnecessary.
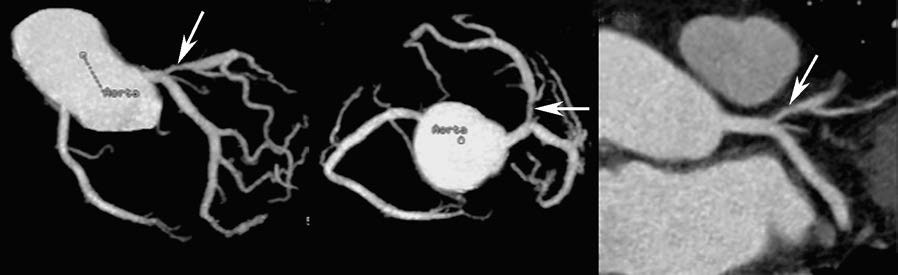
Figure 3 Multislice spiral CT coronary imaging
The arrows indicate a proximal lesion in the left anterior descending artery. The left, middle, and right images show the lesion from different angles.
However, CTA has limitations in accurately assessing the degree of stenosis, especially in the presence of significant calcification. Recently, CT-derived fractional flow reserve (CT-FFR) has been used to assess the functional significance of coronary stenosis. A CT-FFR value <0.80 indicates myocardial ischemia and may warrant further evaluation with coronary angiography to guide treatment strategies.
Echocardiography
Most patients with stable angina have normal resting echocardiograms. In patients with previous myocardial infarction or severe myocardial ischemia, two-dimensional echocardiography may reveal wall motion abnormalities in necrotic or ischemic areas. Stress echocardiography, using exercise or pharmacological stress, can evaluate myocardial perfusion under stress conditions. Echocardiography is also useful in identifying other conditions that may mimic angina caused by coronary artery stenosis, such as hypertrophic obstructive cardiomyopathy or aortic stenosis.
Radionuclide Imaging
Myocardial Perfusion Imaging and Stress Testing
After injection, 201Tl (thallium) is rapidly taken up by normal myocardial cells via coronary blood flow. Resting perfusion defects observed on thallium imaging are typically seen in myocardial scar tissue following infarction. Perfusion defects detected after exercise indicate myocardial ischemia due to insufficient coronary blood supply.
In recent years, 99mTc-MIBI has been used as a substitute for 201Tl in myocardial imaging, making it more feasible for clinical application.
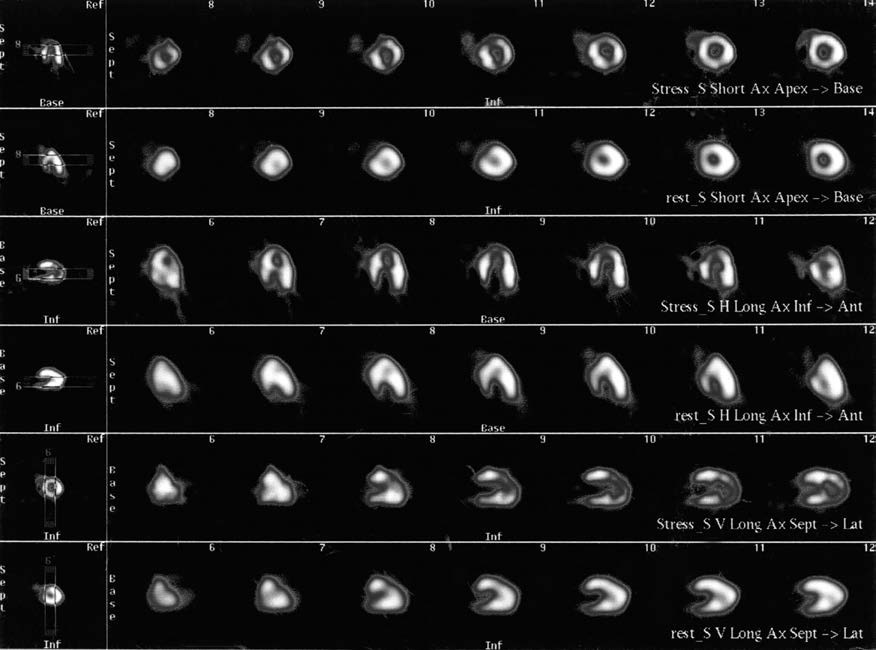
Figure 4 Myocardial perfusion imaging
The first and second rows show short-axis views of the left ventricle (from apex to base, left to right) during stress and rest, respectively. The third and fourth rows show long-axis views of the left ventricle (from the inferior wall to the anterior wall) during stress and rest, respectively. The fifth and sixth rows show vertical long-axis views of the left ventricle (from the septum to the lateral wall) during stress and rest, respectively. The images indicate areas of reduced or absent radiotracer uptake in the anterior wall, apex, and apical inferior wall of the left ventricle during stress, with redistribution and significant radiotracer filling during rest, consistent with myocardial ischemia.
Radionuclide Ventriculography
Using 99mTc-labeled red blood cells, imaging of blood pools within the heart chambers is achieved. By analyzing images captured at different phases of the cardiac cycle, the left ventricular ejection fraction (LVEF) can be measured, and regional wall motion abnormalities in ischemic myocardial areas can be identified.
Positron Emission Tomography (PET)
PET imaging uses positron-emitting radiotracers such as 18F, 11C, and 13N to assess myocardial perfusion and metabolism. This technique not only evaluates myocardial blood flow but also provides insights into myocardial metabolism. By analyzing the match or mismatch between perfusion and metabolic imaging, PET can accurately assess myocardial viability.
Coronary Magnetic Resonance Angiography (CMRA)
CMRA is a novel, non-invasive imaging method for coronary artery assessment that does not involve ionizing radiation. The most used technique involves three-dimensional CMRA obtained with respiratory and electrocardiographic gating. Stress and perfusion MRI images can also reveal myocardial ischemia.
However, limitations such as long imaging times, low spatial resolution, and operator dependency restrict the widespread application of CMRA.
Invasive Tests
Coronary Angiography
Selective coronary angiography remains the gold standard for diagnosing coronary artery disease (CAD). A specially shaped catheter is introduced via the radial artery, femoral artery, or brachial artery to the aortic root, where it is guided into the left and right coronary artery ostia. A small amount of iodine-based contrast agent is injected, and images are captured from various projections. This provides clear visualization of the left and right coronary arteries and their major branches, allowing the identification of stenotic lesions and estimation of their severity. Generally, a reduction in lumen diameter of 70-75% or more is considered to significantly impair blood supply.
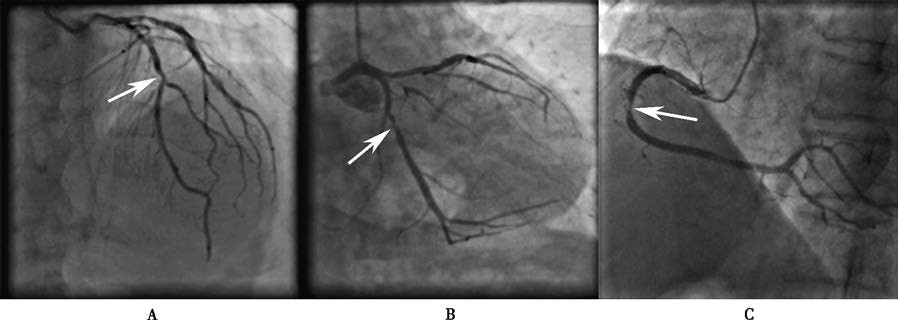
Figure 5 Selective coronary angiography
A. Anteroposterior cranial view (AP + CRA 30°): The arrow indicates a lesion in the mid-segment of the left anterior descending artery.
B. Right anterior oblique caudal view (RAO 30° + CAU 30°): The arrow indicates a lesion in the proximal-to-mid segment of the left circumflex artery.
C. Left anterior oblique view (LAO 45°): The arrow indicates a lesion in the mid-segment of the right coronary artery.
Other Techniques
Intravascular ultrasound (IVUS), optical coherence tomography (OCT), fractional flow reserve (FFR), and quantitative flow ratio (QFR) are additional morphological and functional assessment techniques. These methods are useful for diagnosing CAD and guiding interventional treatments.
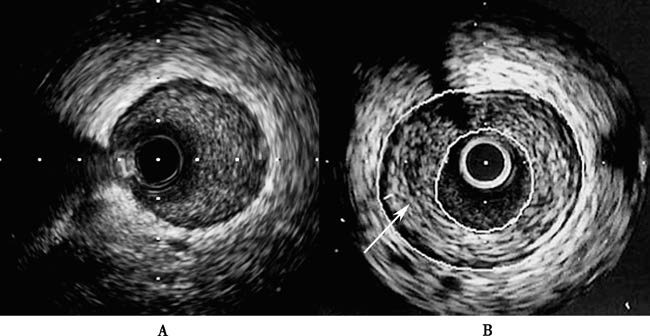
Figure 6 Coronary intravascular ultrasound (IVUS) imaging
A. A segment of a nearly normal vessel.
B. Atherosclerotic lesion in the coronary artery. The arrow indicates a plaque. The inner circle represents the cross-section of the lumen, the outer circle represents the external elastic membrane, and the annular region between the two circles corresponds to the atherosclerotic plaque.
Other Tests
Chest x-rays have no specific diagnostic value for stable angina and are typically normal. However, they can help identify other cardiopulmonary conditions, such as cardiac enlargement or heart failure.
Diagnosis
The diagnosis of stable angina can generally be established based on the characteristic features of angina attacks, combined with the patient’s age and the presence of coronary artery disease risk factors, while excluding other potential causes of chest pain. ECG changes during an angina attack, such as ST-T segment alterations that resolve after the symptoms subside, support the diagnosis of angina. If ECG changes during an attack are not captured, an ECG stress test can be performed. Coronary CT angiography aids in the non-invasive evaluation of coronary artery stenosis and the nature and distribution of arterial wall lesions. Coronary angiography can determine the severity and extent of lesions, and when combined with intravascular imaging and functional assessment techniques, it can assist in diagnosis and guide further treatment.
The Canadian Cardiovascular Society (CCS) classifies the severity of angina into four grades:
Grade I
Ordinary physical activity (e.g., walking or climbing stairs) is not limited, and angina occurs only during strenuous, rapid, or prolonged exertion.
Grade II
Ordinary physical activity is slightly limited. Angina occurs during brisk walking, after meals, in cold or windy conditions, under emotional stress, or within a few hours of waking. Walking more than 200 meters on level ground or climbing more than one flight of stairs is limited.
Grade III
Ordinary physical activity is markedly limited. Angina occurs after walking less than 200 meters on level ground or climbing one flight of stairs.
Grade IV
Angina occurs with minimal activity or at rest.
Differential Diagnosis
Acute Coronary Syndrome (ACS)
Unstable angina shares similar pain location, nature, and ECG changes with stable angina but differs in its triggers. It often occurs at rest or with minimal exertion. Newly developed or significantly worsening exertional angina within one month is also considered unstable angina.
Myocardial infarction is characterized by more severe and prolonged pain (usually lasting more than 30 minutes, sometimes several hours), often accompanied by arrhythmias, heart failure, and/or shock. Sublingual nitroglycerin typically does not relieve the pain.
ECG often shows a typical dynamic evolution. Laboratory tests reveal elevated cardiac biomarkers indicative of myocardial necrosis, along with increased white blood cell counts and erythrocyte sedimentation rates.
Angina caused by Other Conditions
Conditions such as severe aortic stenosis or regurgitation, rheumatic coronary arteritis, syphilitic aortitis leading to coronary ostial stenosis or occlusion, hypertrophic cardiomyopathy, and syndrome X should be differentiated based on clinical manifestations.
Syndrome X is more common in females, with a positive ECG stress test but no stenotic lesions or evidence of coronary spasm on angiography. It is thought to result from coronary microvascular dysfunction and generally has a good prognosis.
Intercostal Neuralgia and Costochondritis
In intercostal neuralgia, pain often involves 1-2 intercostal spaces and is not always confined to the anterior chest. It is sharp or burning, typically continuous rather than episodic, and worsens with coughing, deep breathing, or body movement. Tenderness is present along the affected nerve, and localized pulling pain may occur during arm-raising movements.
In costochondritis, tenderness is localized to the costal cartilage.
Cardiac Neurosis
Patients often report chest pain that is brief (lasting a few seconds) and sharp or persistent (lasting hours) and dull. Pain is typically located near the apex of the heart, below the left breast, or varies in location. Symptoms often appear after fatigue rather than during exertion. Mild physical activity may even provide relief, and patients may tolerate heavy exertion without experiencing chest pain or tightness. Sublingual nitroglycerin is ineffective or only effective after more than 10 minutes. Associated symptoms include palpitations, fatigue, dizziness, insomnia, and other signs of neurosis.
Chest Pain from Other Systemic Diseases
Differentiation is required from conditions such as reflux esophagitis and other esophageal disorders, hiatal hernia, peptic ulcers, intestinal diseases, and cervical spondylosis.
Prognosis
Most patients with stable angina can live for many years, but they remain at risk of acute myocardial infarction or sudden cardiac death. The primary factors determining prognosis are the extent of myocardial blood supply affected by coronary artery disease and cardiac function. Left main coronary artery disease is the most severe, with an annual mortality rate reported to be as high as 30%, followed sequentially by three-vessel, two-vessel, and single-vessel disease. Lesions in the left anterior descending artery generally have a worse prognosis compared to the other two coronary arteries. A reduced ejection fraction and abnormal wall motion, as observed through left ventricular angiography, echocardiography, or radionuclide ventriculography, also carry prognostic significance.
Treatment
The treatment goals are to improve coronary blood supply and reduce myocardial oxygen demand to alleviate symptoms and improve the patient’s quality of life, simultaneously addressing coronary atherosclerosis to prevent myocardial infarction and death, thereby prolonging survival.
Treatment During Episode
Rest
Patients should immediately rest during an angina attack. Symptoms usually subside gradually once physical activity is stopped.
Medication
Fast-acting nitrate preparations can be used. Sublingual tablets or oral sprays act the quickest. For recurrent episodes, intravenous administration may be considered, but the potential for tolerance should be noted. Nitrates not only dilate coronary arteries, reduce resistance, and increase coronary circulation but also dilate peripheral vessels, reducing venous return and lowering both preload and afterload, thereby relieving angina.
Nitroglycerin 0.5 mg sublingually or 1-2 sprays can be administered. Effects begin within 1-2 minutes and last approximately 30 minutes. Delayed or absent response suggests that the patient may not have coronary artery disease or has severe coronary artery disease. Side effects include headache, facial flushing, reflex tachycardia, and hypotension. Orthostatic hypotension may occur with the first dose, so caution is advised.
Isosorbide dinitrate 5-10 mg can be administered sublingually. Effects begin within 2-5 minutes and last 2-3 hours. A spray formulation is also available.
Treatment During the Stable Phase
Lifestyle Adjustments
Patients should:
- Avoid triggering factors as much as possible
- Maintain a light diet and avoid overeating
- Quit smoking and limit alcohol intake
- Reduce mental stress and ensure adequate sleep
- Adjust daily activities and workload to avoid triggering symptoms, while maintaining an appropriate level of physical activity that does not induce pain
Bed rest is generally not necessary.
Medication
β-adrenergic blockers inhibit cardiac β-adrenergic receptors, slowing heart rate, reducing myocardial contractility, lowering blood pressure, and thereby decreasing myocardial oxygen demand. This reduces the frequency of angina attacks and increases exercise tolerance.
Resting heart rate should be reduced to 55-60 beats per minute. In patients with severe angina and no symptoms of bradycardia, the heart rate can be lowered to 50 beats per minute.
Selective β1-receptor blockers without intrinsic sympathomimetic activity are recommended. Dosage should be individualized, starting with a low dose and gradually increasing as needed.
Commonly used β1-receptor blockers include:
- Metoprolol immediate-release tablets, 25-100 mg twice daily
- Metoprolol extended-release tablets, 47.5-190 mg once daily
- Bisoprolol, 5-10 mg once daily
Contraindications include severe bradycardia, high-grade atrioventricular block, sick sinus syndrome, and significant bronchospasm or asthma.
Peripheral vascular disease and severe depression are relative contraindications.
In patients with chronic cor pulmonale, highly selective β1-receptor blockers can be used cautiously.
Commonly used nitrates include isosorbide dinitrate (immediate-release tablets: 5-20 mg, 3-4 times daily; sustained-release tablets: 20-40 mg, 1-2 times daily) and isosorbide mononitrate (immediate-release tablets: 20 mg, twice daily; sustained-release tablets: 40-60 mg, once daily). It is important to ensure a sufficient nitrate-free interval each day to reduce the risk of tolerance. Adverse effects include headache, facial flushing, reflex tachycardia, and hypotension.
Calcium channel blockers (CCBs) block calcium ion entry into cells, inhibiting the excitation-contraction coupling of myocardial cells, thereby reducing myocardial contractility and oxygen consumption. They also dilate coronary arteries, relieve spasms, improve subendocardial myocardial blood flow, and dilate peripheral vessels, lowering arterial pressure and reducing cardiac workload. CCBs improve myocardial microcirculation.
Non-dihydropyridine CCBs include verapamil (immediate-release tablets: 40-80 mg, 3 times daily; sustained-release tablets: 240 mg, once daily) and diltiazem (immediate-release tablets: 30-60 mg, 3 times daily; sustained-release tablets: 90 mg, once daily). Both drugs have negative inotropic and negative chronotropic effects. Caution is required when combining these with β-blockers.
Dihydropyridine CCBs include nifedipine (controlled-release tablets: 30 mg, once daily) and amlodipine (5-10 mg, once daily). These are more suitable for patients with concomitant hypertension.
Common side effects of CCBs include peripheral edema, constipation, palpitations, and facial flushing. Other adverse effects may include headache, dizziness, and weakness. Diltiazem and verapamil can slow the sinus node rate and atrioventricular conduction and suppress myocardial contractility. Therefore, they should not be used in patients with severe bradycardia, high-grade atrioventricular block, or sick sinus syndrome. They are also not recommended for patients with left ventricular dysfunction.
Other medications are primarily used when β-blockers or CCBs are contraindicated, poorly tolerated, or fail to control symptoms.
Trimetazidine (immediate-release tablets: 20-60 mg, 3 times daily; sustained-release tablets: 35 mg, twice daily) inhibits fatty acid oxidation and enhances glucose metabolism, improving oxygen utilization to treat myocardial ischemia.
Nicorandil (5 mg, 3 times daily), an ATP-dependent potassium channel opener with pharmacological properties similar to nitrates. dilates microvessels.
Ivabradine (5-7.5 mg, twice daily), the first selective inhibitor of the sinus node If current, is used to slow sinus heart rate in stable angina.
Ranolazine inhibits late sodium currents in myocardial cells, preventing calcium overload and improving myocardial metabolic activity.
Cyclooxygenase (COX) inhibitors block thromboxane A2 synthesis, thereby inhibiting platelet aggregation. This includes irreversible COX inhibitors (e.g., aspirin) and reversible COX inhibitors (e.g., indobufen).
Aspirin, the cornerstone of antiplatelet therapy, is recommended for all patients without contraindications. The optimal dose is 75-150 mg daily. The main adverse effects are gastrointestinal hemorrhage or allergic reactions to aspirin.
Indobufen is a reversible COX-1 inhibitor that also reduces platelet factors 3 and 4, decreasing platelet aggregation. It has a lower inhibition rate of prostaglandins, resulting in fewer gastrointestinal side effects and lower hemorrhage risks. It is suitable for patients at risk of hemorrhage or gastrointestinal damage. The maintenance dose is 100 mg, twice daily.
P2Y12 receptor antagonists inhibit ADP-induced platelet activation. Commonly used agents in clinical practice include clopidogrel and ticagrelor.
Clopidogrel is a second-generation P2Y12 receptor antagonist that is a prodrug. It requires hepatic metabolism via the cytochrome P450 (CYP450) enzyme system, specifically CYP2C19, to convert into its active metabolite, irreversibly inhibiting the P2Y12 receptor and platelet aggregation. It is primarily used in patients with stent implantation or those with contraindications to aspirin. The typical maintenance dose is 75 mg daily.
Patients with the CYP2C19 slow-metabolizer genotype may have reduced antiplatelet effects with clopidogrel.
To lower LDL-C, statins are the first choice. They inhibit HMG-CoA reductase, the rate-limiting enzyme in cholesterol synthesis in liver cells, reducing intracellular cholesterol levels and increasing the expression of LDL receptors on the hepatocyte membrane. This effectively lowers total cholesterol (TC) and low-density lipoprotein cholesterol, slows plaque progression, and stabilizes plaques. All patients with confirmed coronary artery disease, regardless of their baseline lipid levels, should receive statin therapy to reduce LDL-C levels to below 1.8 mmol/L (70 mg/dL).
Commonly used statins include:
- Atorvastatin (10-80 mg, once nightly)
- Rosuvastatin (5-20 mg, once nightly)
- Pitavastatin (1-2 mg, once nightly)
- Pravastatin (20-40 mg, once nightly)
- Fluvastatin (40-80 mg, once nightly)
- Simvastatin (20-40 mg, once nightly)
Statins are generally very safe, but liver enzymes (e.g., ALT) and creatine kinase (CK) levels should be monitored to detect potential liver damage or muscle injury caused by the medication, especially during high-dose intensive lipid-lowering therapy.
Cholesterol absorption inhibitors selectively inhibit intestinal cholesterol transport proteins, effectively reducing intestinal cholesterol absorption, plasma cholesterol levels, and hepatic cholesterol stores. They can be used in combination with statins for patients whose cholesterol levels remain uncontrolled or who cannot tolerate high-dose statins. Common drugs include ezetimibe (10 mg, once daily) and alipogene tiparvovec (10 mg, once daily).
PCSK9 inhibitors increase LDL receptor recycling on hepatocytes, thereby enhancing LDL clearance and lowering LDL-C levels. Indications for PCSK9 inhibitors include heterozygous familial hypercholesterolemia or patients with atherosclerotic cardiovascular disease (ASCVD) who require further LDL-C reduction despite dietary control and maximum tolerated statin therapy.
Commonly used drugs include:
- Evolocumab (140 mg subcutaneously every 2 weeks)
- Alirocumab (75 mg subcutaneously every 2 weeks)
- Toripalimab (150 mg subcutaneously every 2 weeks)
Inclisiran is a small interfering RNA (siRNA) drug that targets PCSK9 mRNA in the liver, blocking PCSK9 protein synthesis upstream. It can be administered as a subcutaneous injection once every 6 months.
In addition to strict lifestyle modifications, fibrates (e.g., fenofibrate, 200 mg once daily) or prescription-grade omega-3 fatty acids (e.g., eicosapentaenoic acid, 2 g twice daily) can be initiated for treatment.
Angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and angiotensin receptor-neprilysin inhibitors (ARNIs) significantly reduce the relative risk of major cardiovascular events, such as cardiovascular death and non-fatal myocardial infarction, in patients with coronary artery disease. ACEIs are recommended for high-risk patients with stable angina combined with hypertension, diabetes, heart failure, or left ventricular systolic dysfunction.
Commonly used ACEIs include:
- Captopril (12.5-50 mg, 3 times daily)
- Enalapril (5-10 mg, 2 times daily)
- Perindopril (4-8 mg, once daily)
- Ramipril (5-10 mg, once daily)
- Benazepril (10-20 mg, once daily)
- Lisinopril (10-20 mg, once daily)
-
For patients intolerant to ACEIs, ARBs or ARNIs can be used as alternatives.
For patients with stable angina following myocardial infarction, beta blockers can reduce the incidence of cardiovascular events.
3) Revascularization Therapy
The decision to pursue conservative medical therapy or revascularization (including percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG]) should be based on the patient’s clinical characteristics, objective evidence of myocardial ischemia, coronary lesion anatomy, and the surgical experience of the local medical center. For patients with stable angina, only revascularization of ischemia-causing lesions provides clinical benefit.
Percutaneous coronary intervention (PCI) includes percutaneous balloon angioplasty, coronary stent implantation, plaque atherectomy, intracoronary laser therapy, and shockwave balloon therapy. Compared to medical therapy alone, PCI can improve quality of life (e.g., increase exercise tolerance), but it does not significantly reduce the incidence of myocardial infarction or mortality. The main factors affecting PCI efficacy are in-stent restenosis and in-stent thrombosis.
With advancements in technology, particularly new drug-eluting stents and antiplatelet medications, PCI outcomes have continued to improve. In addition to metallic drug-eluting stents, biodegradable stents and drug-coated balloons can achieve similar efficacy in appropriately selected patients while avoiding the long-term presence of foreign material in the coronary arteries.
In cases without clinical evidence of ischemia, physiological assessment techniques such as fractional flow reserve (FFR) or quantitative flow ratio (QFR) are recommended to evaluate the functional significance of borderline lesions. Lesions with evidence of ischemia (FFR or QFR < 0.80) may be considered for interventional treatment.
Coronary artery bypass grafting (CABG) involves using the patient’s own great saphenous vein or radial artery as bypass graft material. One end of the graft is anastomosed to the aorta, and the other end is connected to the distal segment of the diseased coronary artery. Alternatively, the left internal mammary artery can be used as a free graft and anastomosed to the distal segment of the diseased left anterior descending artery to improve blood flow supply to the myocardium served by the diseased coronary artery.
After surgery, CABG significantly alleviates angina symptoms and improves the patient’s quality of life. However, CABG is relatively more invasive. Despite advancements in surgical techniques and equipment that have greatly improved success rates, the perioperative mortality rate remains higher than that of PCI, ranging from 1% to 4%, depending on the experience of the medical center. This rate is also influenced by the patient’s preoperative coronary lesion severity, cardiac function, and the presence of other complications. Additionally, grafted vessels may become occluded over time. Therefore, the risks and benefits should be carefully weighed on an individual basis, and surgical indications should be chosen cautiously.
The choice between PCI and CABG for patients requiring revascularization depends on the anatomical characteristics of the coronary lesions, the patient’s tolerance for open-heart surgery, and the patient’s preferences. For patients who can tolerate open-heart surgery, CABG is the preferred option for those with left main coronary artery disease combined with two or more diseased coronary vessels (particularly in cases with high lesion complexity scores, such as a high SYNTAX score), multivessel disease with diabetes, or lesions with severe tortuosity and heavy calcification.
Prevention
For stable angina, in addition to using medications to prevent recurrent angina attacks, comprehensive strategies should focus on halting or reversing the progression of atherosclerosis and preventing myocardial infarction to improve prognosis. The ABCDE approach provides guidance for secondary prevention:
- A: Antiplatelet therapy, anti-anginal treatment, and the use of ACEIs/ARBs
- B: Beta blockers and blood pressure control
- C: Cholesterol management and smoking cessation
- D: Dietary control and diabetes management
- E: Education on healthy lifestyles and exercise