Under normal circumstances, the heart beats rhythmically within a certain range of frequency. These impulses originate from the sinoatrial node (SAN) and are conducted in a specific sequence and frequency to the atria and ventricles, coordinating synchronous contraction of the heart chambers to produce a heartbeat. This process repeats continuously, forming a normal rhythm. Cardiac arrhythmia is abnormalities in the frequency, rhythm, origin, conduction speed, or sequence of cardiac impulses. Arrhythmias can occur under physiological conditions but are more commonly seen in pathological states, including both cardiac and non-cardiac diseases.
Cardiac Conduction System
The cardiac conduction system is composed of specialized myocardial tissue responsible for generating and conducting normal electrical impulses. It includes the sinoatrial node, internodal tracts, atrioventricular (AV) node, His bundle, left and right bundle branches, and Purkinje fibers.
The SAN is the pacemaker of the heart, responsible for generating the normal sinus rhythm. It is located at the junction of the superior vena cava and the posterior wall of the right atrium, spindle-shaped, 10 - 20 mm in length and 2 - 3 mm in width, and lies less than 1 mm beneath the epicardium. The SAN is primarily composed of P (pacemaker) cells and T (transitional) cells. The normal pacing rate of the SAN is 60 - 100 beats per minute. After impulse formation in the P cells, the impulse is conducted through the T cells to the atrial tissue outside the SAN. The blood supply to the SAN originates from the right coronary artery in 55-60% of cases and from the left circumflex artery in 40-45% of cases.
The internodal tracts connect the SAN to the AV node and are divided into anterior, middle, and posterior tracts. The anterior internodal tract gives off a branch to the left atrium, known as the interatrial tract or Bachmann's bundle.
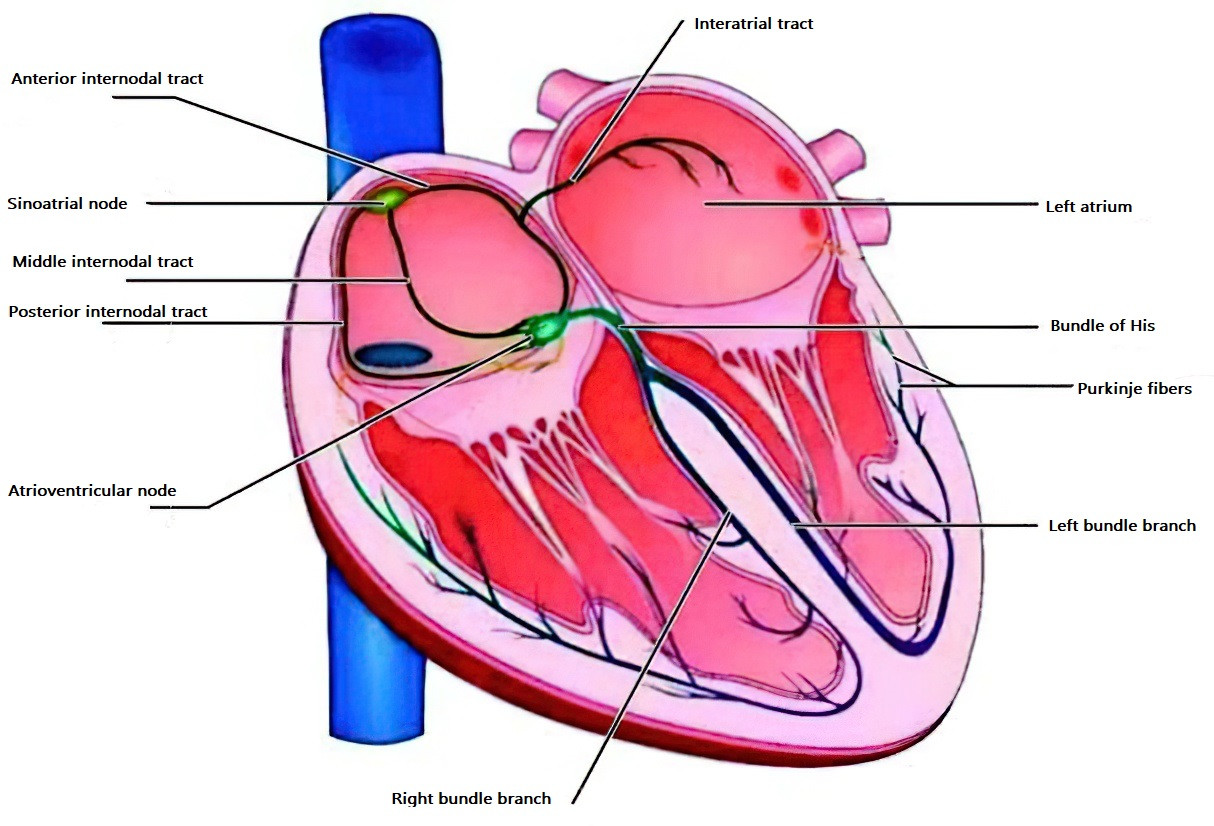
Figure 1 Diagram of the cardiac conduction system
The AV node serves as the central relay station of the cardiac conduction system, facilitating impulse transmission from the atria to the ventricles. The upper part of the AV node is composed of transitional cells that connect with atrial muscle; the middle part is the compact zone with interwoven muscle fibers; and the lower part consists of longitudinally arranged fibers that extend into the His bundle. The AV node is the most important secondary pacemaker, with a pacing rate of 40-60 beats per minute. The blood supply to the AV node is typically provided by the right coronary artery in 85-90% of cases, with the remaining supplied by the circumflex artery.
The His bundle is a cord-like structure, 15-20 mm in length, originating from the anteroinferior margin of the AV node. It is encased in a fibrous sheath and traverses the central fibrous body, running along the crest of the interventricular septum before dividing into the left and right bundle branches.
The left bundle branch further divides into the left anterior and left posterior fascicles, which supply the two groups of papillary muscles. The left bundle branch reaches the left ventricular surface of the interventricular septum first, making this region the earliest activated part of the ventricles.
The right bundle branch travels along the right side of the interventricular septum and extends to the base of the anterior papillary muscle, where it branches into smaller fibers. Its main trunk is thin and long, making it susceptible to damage and conduction block.
The terminal portions of the left and right bundle branches branch out into a network of Purkinje fibers, which lie beneath the endocardium and innervate all ventricular myocardial cells. The blood supply to these structures is derived from the left anterior descending artery and the posterior descending artery of the right coronary artery.
The sequence of normal electrical activity begins with impulse generation in the SAN. The impulse is transmitted via the internodal tracts, the interatrial tract, and ordinary atrial muscle to the left atrium and AV node. Within the AV node, conduction slows significantly, creating a physiological AV delay. After reaching the His bundle, conduction accelerates. The conduction speed through the bundle branches and Purkinje fibers is extremely rapid, ensuring nearly simultaneous activation of the entire ventricular myocardium. Finally, the impulse reaches the epicardium, completing a cardiac cycle.
The cardiac conduction system is regulated by both the vagus nerve and the sympathetic nervous system. Excitation of the vagus nerve inhibits the automaticity and conductivity of the SAN, prolongs the refractory period of the SAN and surrounding tissues, slows conduction through the AV node, and extends its refractory period. The effects of the sympathetic nervous system are opposite to those of the vagus nerve.
##Etiology
The causes of cardiac arrhythmia can be classified into genetic and acquired factors.
Genetic arrhythmias are often caused by gene mutations leading to ion channelopathies, which result in abnormal ion flow in myocardial cells. Currently identified genetic arrhythmias include long QT syndrome, short QT syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia (CPVT), and early repolarization syndrome. Some cases of atrial fibrillation (such as isolated or familial atrial fibrillation) and Wolff-Parkinson-White syndrome are also associated with specific gene mutations. Additionally, conditions such as progressive cardiac conduction disease, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy (ARVC), left ventricular non-compaction cardiomyopathy, idiopathic ventricular fibrillation, and arrhythmia-related sudden death syndromes are linked to genetic factors.
For patients clinically diagnosed or suspected of having genetic arrhythmias, especially survivors of sudden cardiac death and their first-degree relatives, genetic testing and risk assessment are recommended.
Acquired arrhythmias can result from physiological or pathological factors.
Exercise, emotional changes, or other factors that stimulate the sympathetic nervous system can lead to tachyarrhythmias, while vagal stimulation during sleep or relaxation may cause bradyarrhythmias. Normally, the sympathetic and vagal nervous systems maintain a balance, but when this balance is disrupted, various types of tachyarrhythmias or bradyarrhythmias can occur.
Pathological factors can be further divided into cardiac, systemic, and other organ-related causes.
Cardiac causes primarily include structural heart diseases such as coronary artery disease, hypertensive heart disease, valvular heart disease, cardiomyopathy, myocarditis, infective endocarditis, and congenital heart disease.
Systemic causes include drug toxicity, electrolyte and acid-base imbalances, and dysregulation of neurohumoral functions.
Functional or structural changes in other organs, such as hyperthyroidism, anemia, severe infections, and stroke, can also trigger arrhythmias.
Additionally, arrhythmias may be induced by chest surgery (especially cardiac surgery), general anesthesia, and various cardiac interventional procedures.
Classification
Cardiac arrhythmias can be classified based on location, mechanism, and heart rate.
Classification by location:
- Supraventricular arrhythmias (including sinus, atrial, and atrioventricular junctional arrhythmias)
- Ventricular arrhythmias
Classification by mechanism:
- Abnormal impulse formation
- Abnormal impulse conduction
Classification by heart rate:
- Tachyarrhythmias (fast arrhythmias)
- Bradyarrhythmias (slow arrhythmias)
Abnormal impulse formation
Sinus arrhythmias:
- Sinus tachycardia
- Sinus bradycardia
- Sinus arrhythmia
- Sinus arrest and sick sinus syndrome
Ectopic Rhythms
Active ectopic rhythms:
- Premature beats (atrial, junctional, and ventricular)
- Paroxysmal tachycardia (atrial, junctional, atrioventricular reentrant, and ventricular) and non-paroxysmal tachycardia
- Atrial flutter and atrial fibrillation
- Ventricular flutter and ventricular fibrillation
Passive ectopic rhythms:
- Atrial escape beats and atrial escape rhythm (rare)
- Junctional escape beats and junctional escape rhythm
- Ventricular escape beats and ventricular escape rhythm
-
Abnormal Impulse Conduction
Physiological conduction abnormalities include interference and interference-related atrioventricular dissociation.
Conduction blocks:
- Sinoatrial block
- Intra-atrial and interatrial conduction block
- Atrioventricular block (first-degree, second-degree, and third-degree AV block)
- Intraventricular conduction block (left bundle branch, right bundle branch, and fascicular blocks)
Reentry and accessory pathway abnormalities:
- Atrioventricular nodal reentrant tachycardia (AVNRT) and intraventricular reentrant tachycardia
- Atrioventricular reentrant tachycardia (AVRT) with accessory pathways, ventricular preexcitation, and short PR syndrome
Coexistence of Abnormal Impulse Formation and Conduction
This includes repetitive rhythms and parasystole, and the most common is ventricular parasystole.
Arrhythmias Involving Artificial Pacemakers
These include interactions between the pacing modes (e.g., DDD(R) and VVI(R) pacemakers), pacing cycles, sensing, and intrinsic rhythms.
Mechanisms of Cardiac Arrhythmias
The mechanisms of cardiac arrhythmias involve abnormal impulse formation and/or abnormal impulse conduction.
Abnormal Impulse Formation
Abnormal impulse formation includes abnormal automaticity and triggered activity.
Abnormal automaticity is inappropriate impulse generation by myocardial cells with intrinsic automaticity (e.g., sinoatrial node, internodal tracts, atrioventricular node, and His-Purkinje fibers) due to changes in autonomic nervous system excitability or intrinsic pathological changes. Alternatively, myocardial cells without intrinsic automaticity, such as atrial and ventricular myocytes, may develop abnormal automaticity under pathological conditions (e.g., myocardial ischemia, drug effects, electrolyte imbalances, or elevated catecholamines).
Abnormal automaticity of normal pacemaker sites results from inappropriate impulse generation. Abnormal automaticity at ectopic sites occurs when non-pacemaker cells gain automaticity.
Abnormal automaticity can lead to two types of arrhythmias:
- Active ectopic rhythms
- Passive ectopic rhythms
Active ectopic rhythms occur when the ectopic pacemaker rate exceeds that of the sinoatrial node, dominating the heart's rhythm. Examples include premature beats or automatic tachycardia.
Passive ectopic rhythms occur when the sinoatrial node rate slows or impulse propagation is blocked, allowing ectopic impulses to capture the ventricles. Examples include escape beats or escape rhythms.
Triggered activity is oscillations in membrane potential (known as afterdepolarizations) that occur during or after repolarization of the action potential in atria, ventricles, or His-Purkinje fibers. When these oscillations reach the threshold potential, they can trigger new depolarizations and excitatory responses, leading to triggered activity. Sustained repetitive triggered activity can result in tachyarrhythmias.
Triggered activity can be observed in conditions such as elevated catecholamine levels, myocardial ischemia-reperfusion, hypokalemia, hypercalcemia, and digitalis toxicity.
Afterdepolarizations are classified into early afterdepolarizations and late/delayed afterdepolarizations.
Early afterdepolarizations (EADs) occur during phase 2 or phase 3 of the action potential and are primarily associated with inward calcium currents (Ica).
Late/delayed afterdepolarizations (DADs) occur during phase 4 of the action potential and are mainly associated with oscillations in intracellular calcium concentrations.
Abnormal Impulse Conduction
Abnormal impulse conduction includes reentry, conduction block, and abnormal conduction.
Reentry is the most common mechanism of tachyarrhythmias. The three essential conditions for the formation and maintenance of reentry are the reentry circuit, unidirectional conduction block, and slow conduction. At this point, the conduction properties and refractory periods in different areas of the heart vary. This includes the fast pathway (β pathway), which has fast conduction and a long refractory period, and the slow pathway (α pathway), which has slow conduction and a short refractory period. The fast and slow pathways are connected to form a closed loop. In certain conditions, such as with premature beats, one of the pathways may undergo unidirectional conduction block because it is still in the refractory period following the previous activation. The excitation from the premature beat then propagates along the other pathway with slow conduction. If the slow conduction is sufficiently long, the pathway that was previously in the refractory period will recover excitability, and the excitation can return along that pathway to form a reentrant circuit. The impulse will cycle repeatedly within the loop, resulting in sustained tachyarrhythmias. A characteristic feature of reentry-induced tachycardia is its sudden onset and termination, often triggered by a premature beat, and it can also be terminated by premature beats or rapid pacing. Reentry can be classified as micro-reentry or macro-reentry. The former includes small-scale reentries within the atrioventricular node, atria, or between Purkinje fibers and ventricular muscle, while the latter includes macro-reentries such as those between the atrium and ventricle or between the bundle branches. It is currently believed that the histological basis of reentry includes both anatomical reentry (such as reentry involving accessory pathways) and functional reentry. The latter does not have anatomical limitations and can occur in adjacent fibrous tissues with different electrophysiological properties. These tissues' excitability, refractory periods, and the anisotropy of intercellular resistance allow reentry to initiate and sustain. Moreover, the functional heterogeneity of myocardial electrophysiology may be either fixed or dynamically changing, and this could be the pathological basis for tachycardia and fibrillation.
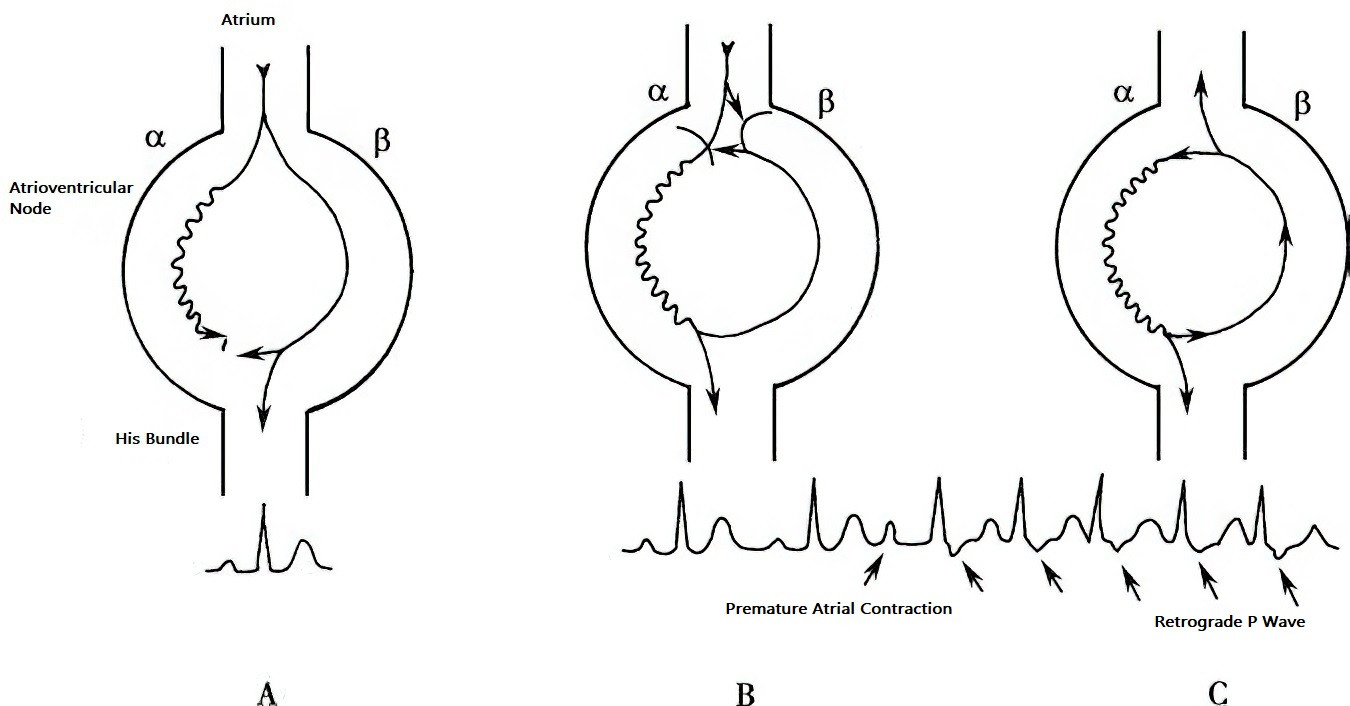
Figure 2 Schematic diagram of atrioventricular nodal reentry
The figure illustrates α and β pathways within the atrioventricular (AV) node. The α pathway has slow conduction velocity and a short refractory period. The β pathway has fast conduction velocity and a long refractory period. A. During sinus rhythm, the impulse travels anterogradely through the β pathway to the ventricles, resulting in a normal PR interval. Simultaneously, the impulse also travels anterogradely through the α pathway but is blocked due to encountering the refractory period, preventing it from reaching the His bundle. B. During a premature atrial contraction (PAC), the impulse is blocked in the β pathway but conducts slowly through the α pathway to the ventricles, leading to a prolonged PR interval. Due to the slow conduction, the β pathway has sufficient time to recover excitability, allowing the impulse to conduct retrogradely through the β pathway back to the atrium. This completes a single reentry circuit, producing a retrograde P wave (atrial echo). C. The atrial echo then conducts anterogradely again through the α pathway, sustaining the reentry circuit and causing atrioventricular nodal reentrant tachycardia (AVNRT).
Conduction block occurs when an impulse encounters myocardial tissue in a refractory state, resulting in either physiological block or pathological block. Physiological block results from normal refractory periods or interference phenomena, while pathological block results from abnormal conduction properties unrelated to normal refractoriness.
Abnormal conduction primarily involves accessory pathways, which provide alternative routes for impulse propagation. Atrioventricular accessory pathways are the most common, but other rare pathways include atrium-His bundle, atrioventricular node-ventricular fibers, and fascicle-ventricular fibers. Impulses from the sinus or atrial pacemakers may travel prematurely through accessory pathways to the ventricles, causing ventricular preexcitation. Reentry between accessory pathways and normal AV conduction pathways can lead to atrioventricular reentrant tachycardia (AVRT).
Diagnosis
Medical History
The diagnosis of cardiac arrhythmias begins with a thorough collection of the patient's medical history. Patients should be encouraged to objectively describe their symptoms, such as palpitations, and the sensations they experience during episodes. The medical history often provides valuable clues for diagnosis. Key aspects to inquire about include:
- Triggers and frequency of episodes, onset and termination patterns, symptoms, and signs during episodes
- History of similar arrhythmia episodes in the past and whether there is a family history of similar conditions
- History of known cardiac diseases
- Presence of systemic diseases that may cause cardiac abnormalities, such as hyperthyroidism
- Medication history, especially the use of antiarrhythmic drugs, digitalis glycosides, or medications that affect electrolyte balance
- Presence of implanted devices, such as permanent cardiac pacemakers
Physical Examination
The primary focus of the physical examination is to determine whether cardiovascular disease is present.
Assessing heart rate and rhythm can help identify arrhythmias such as premature beats, atrial fibrillation, tachycardia, or bradycardia. In cases of complete atrioventricular block or AV dissociation, the heart rhythm may appear regular, but the intensity of the first heart sound varies due to different PR intervals. Left bundle branch block may be associated with paradoxical splitting of the second heart sound.
Electrocardiographic (ECG) Examination
Resting ECG
Resting ECG is the most important non-invasive diagnostic tool for arrhythmias. The following principles guide ECG analysis:
- Assessing the P-wave morphology to determine whether the rhythm is sinus or ectopic
- Measuring the P-P or R-R intervals to calculate atrial or ventricular rates and assess for tachycardia, bradycardia, or irregular rhythms
- Measuring the PR and QT intervals to evaluate for prolongation or shortening
- Comparing the P-P interval with the R-R interval to assess the relationship between atrial and ventricular rhythms
- Analyzing waveform characteristics across leads, including changes in ST-T segments, to identify arrhythmia types and myocardial ischemia
Resting ECG can also detect:
- Delta waves in Wolff-Parkinson-White syndrome
- ST-segment abnormalities in right precordial leads characteristic of Brugada syndrome
- Epsilon waves in arrhythmogenic right ventricular cardiomyopathy
Emerging technologies, such as high-frequency QRS (Hyper Q) analysis, use high-frequency filters (150-250 Hz) to extract QRS high-frequency signals. By analyzing signal frequency, amplitude, and morphology, this method provides additional cardiac electrophysiological information. It complements conventional ECG in assessing ST-T changes for myocardial ischemia, aids in coronary artery disease screening and risk stratification, and helps identify individuals at risk for sudden cardiac death.
Signal-averaged ECG (SAECG) amplifies subtle variations in surface ECG signals using signal processing techniques. It is commonly used to detect ventricular late potentials, which are low-amplitude signals at the terminal part of the QRS complex. These indicate delayed ventricular activation and are associated with an increased risk of ventricular arrhythmias, particularly after myocardial infarction.
Exercise ECG
Exercise ECG testing is widely used as a stress test. In addition to detecting myocardial ischemia caused by coronary artery disease and assessing prognosis, it is also used to:
- Determine whether myocardial ischemia is associated with arrhythmias
- Evaluate the risk of exercise-induced ventricular arrhythmias (e.g., catecholamine-sensitive ventricular tachycardia)
- Assess patients with known or suspected ventricular preexcitation. For example, during sinus rhythm, if conduction through an overt accessory pathway disappears suddenly during exercise, it suggests a low risk of rapid conduction and life-threatening ventricular arrhythmias during atrial fibrillation
- Evaluate the efficacy of medications or catheter ablation in patients with exercise-induced ventricular arrhythmias
Premature beats and tachycardia (e.g., atrial premature beats, ventricular premature beats, or atrial tachycardia) may occur during exercise testing in healthy individuals.
Continuous ECG Monitoring
Continuous ECG monitoring is commonly used to screen for and diagnose arrhythmias. It includes:
- Holter ECG monitoring
- Event recorders
- Wearable ECG monitors
- Insertable cardiac monitors
Holter ECG monitoring is a portable device recording ECG continuously for 24-72 hours. It monitors arrhythmias and myocardial ischemia during daily activities, evaluates symptoms like palpitations or syncope for arrhythmia correlation, and assesses the relationship between arrhythmia or ischemia episodes and daily activities. Holter monitoring also provides data on circadian distribution, heart rate variability, QT interval variability, and the efficacy of antiarrhythmic drugs, pacemakers, or implantable cardioverter-defibrillators.
Event recorders are suitable for infrequent arrhythmias, and these devices can be carried for up to 30 days. They record ECG during arrhythmic episodes and transmit data via wired or wireless networks for arrhythmia diagnosis and analysis.
Recent developments in wearable devices allow real-time ECG recording via 4G or 5G networks. These devices store data in the cloud and can theoretically provide indefinite long-term ECG monitoring.
Insertable cardiac monitors (ICMs) are small, implantable, invasive ECG monitoring devices placed subcutaneously. They are easy to implant, have a lifespan of up to three years, and provide precise signal acquisition with remote monitoring capabilities. ICMs facilitate the diagnosis and follow-up of arrhythmias, particularly in cases of recurrent unexplained syncope or for monitoring and managing atrial fibrillation.
Transesophageal Cardiac Electrophysiological Study
Transesophageal cardiac electrophysiological study, also known as transesophageal atrial pacing, utilizes the anatomical proximity of the posterior wall of the left atrium to the esophagus. By inserting an esophageal electrode through the nasal cavity into the esophagus at the atrial level, electrical activity of the atrium and ventricle (i.e., esophageal ECG) can be recorded, and rapid atrial pacing or programmed electrical stimulation can be performed.
Esophageal ECG provides a clear view of atrial and ventricular electrical activity, allowing the determination of the relationship between atrioventricular electrical activity, differentiation of types of supraventricular tachycardia, and distinction between wide-QRS supraventricular tachycardia and ventricular tachycardia. Esophageal rapid atrial pacing can make preexcitation patterns more distinct, aiding in the diagnosis of atypical Wolff-Parkinson-White syndrome. Electrical stimulation can induce and terminate tachycardia, evaluate sinoatrial node function, and terminate certain reentrant supraventricular tachycardias that are resistant to medication.
This examination is simple, safe, and easy to perform. However, with the widespread adoption of intracardiac electrophysiological studies and other advanced techniques, its clinical use has become less frequent.

Figure 3 Termination of supraventricular tachycardia by rapid atrial pacing via esophageal electrode
The figure shows a case of supraventricular tachycardia (SVT) with a heart rate of 166 beats per minute. After delivering rapid atrial pacing signals (at a frequency of 220 beats per minute) via an esophageal electrode, the tachycardia is successfully terminated.
Intracardiac Electrophysiological Study (EPS)
Intracardiac EPS involves placing multiple electrode catheters through veins and/or arteries into different intracardiac locations. Using a multichannel physiological recorder (8-12 channels or more), it synchronously records electrical activity from various sites, including the high right atrium, His bundle, coronary sinus (reflecting left atrial and left ventricular electrical activity), and right ventricle. Programmed electrical stimulation and rapid atrial or ventricular pacing can also be performed to assess the electrophysiological properties of different cardiac tissues.
Applications of intracardiac EPS include:
- Diagnostic applications
- Therapeutic application
- Prognostic assessment
Diagnostic applications:
- Confirming the presence and type of arrhythmias
- Identifying the origin and mechanism of arrhythmias
Therapeutic applications:
- Terminating tachycardia episodes using electrical stimulation
- Evaluating the efficacy of treatments in preventing tachycardia induced by electrical stimulation
- Assessing the ability of implanted devices to correctly detect and terminate tachycardia induced by electrical stimulation
- Ablating myocardial tissue involved in tachycardia pathways using various energy sources (e.g., radiofrequency, cryotherapy, ultrasound) via electrode catheters, thereby curing tachycardia (catheter ablation)
Prognostic assessment:
- Determining susceptibility to ventricular tachycardia through electrical stimulation
- Assessing the risk of sudden cardiac death
Common indications for intracardiac EPS include:
- Sinoatrial node function assessment
- Atrioventricular conduction and intraventricular conduction block
- Tachycardias
- Unexplained syncope
- Diagnostic drug testing
Sinoatrial Node Function Assessment
For patients with suspected sick sinus syndrome (SSS) but inconclusive ECG evidence, intracardiac EPS can help confirm the diagnosis.
Measurements include:
- Sinus node recovery time (SNRT): Normal SNRT <1500 ms, SNRT >1600 ms suggesting possible SSS, while SNRT >2000 ms confirming the diagnosis
- Sinoatrial conduction time (SACT): This evaluating sinoatrial node dysfunction under variable conditions
Atrioventricular Conduction and Intraventricular Conduction Block
First-degree or second-degree type I atrioventricular (AV) block typically occurs at the AV node, while second-degree type II AV block commonly occurs at the His bundle. Surface ECG often cannot accurately localize AV or intraventricular conduction blocks, but electrophysiological studies can pinpoint the exact site of the block.
Key assessments include:
- The maximum atrial pacing rate that the AV node can sustain with 1:1 conduction (normal ≥130 bpm)
- Refractory periods of the AV node and His-Purkinje system using programmed atrial stimulation
- Conduction intervals such as PA (reflecting intra-atrial conduction), AH (reflecting AV nodal conduction), and HV (reflecting His-Purkinje conduction)
- Prolonged HV intervals (>80 ms) in intraventricular block suggesting a high risk of complete AV block
Tachycardias
Intracardiac EPS can elucidate the mechanisms of tachycardia. For example, atrioventricular nodal reentrant tachycardia (AVNRT) involves dual or multiple reentrant pathways, with programmed stimulation showing a characteristic jump phenomenon (sudden AH prolongation >50 ms, indicating conduction switching from a fast to a slow pathway).
Indications for intracardiac EPS in tachycardia include:
- Recurrent supraventricular or ventricular tachycardia with significant symptoms
- Infrequent episodes that are difficult to diagnose
- Difficulty distinguishing supraventricular tachycardia with aberrant conduction from ventricular tachycardia
- Conducting electrophysiological-pharmacological tests to evaluate antiarrhythmic drug efficacy or assess non-pharmacological treatments
- Endocardial mapping to localize the origin of tachycardia and perform catheter ablation simultaneously
Unexplained Syncope
For patients with unexplained syncope after comprehensive history-taking, physical examination, and non-invasive cardiac tests, intracardiac EPS may be considered.
Diagnostic Drug Testing
Common drug tests include atropine, isoproterenol, and ATP tests.
Atropine and isoproterenol tests are used to diagnose sick sinus syndrome, localize and characterize AV conduction block, and evaluate the efficacy of catheter ablation or provoke tachycardia.
ATP tests are often used to terminate ongoing supraventricular tachycardia or identify concealed accessory pathways.
Three-dimensional Cardiac Electrophysiological Mapping System
Conventional intracardiac electrophysiological mapping relies on digital subtraction angiography (DSA) imaging, which lacks spatial accuracy for complex arrhythmias, resulting in lower surgical success rates, prolonged procedure times, and extended x-ray exposure. The three-dimensional (3D) cardiac mapping system is a rapidly evolving and widely adopted technology that offers significant advantages, including enhanced visualization, higher mapping efficiency and safety, reduced radiation exposure, and a shorter learning curve. It has become an essential tool in catheter ablation for all types of complex arrhythmias.
The most used 3D mapping systems in clinical practice are the Carto and EnSite systems.
The Carto 3D mapping system uses magnetic field-based positioning to generate a stable 3D electroanatomical map of the heart. The EnSite 3D mapping system employs electric field-based positioning to provide precise voltage mapping of the heart. With advancements in technology, the latest generations of both Carto and EnSite systems now integrate magnetic and electric field positioning methods. This dual-mode approach enables the construction of more stable and accurate 3D electroanatomical maps. Additionally, these systems can merge 3D electroanatomical maps with 3D anatomical images of cardiac chambers and vasculature obtained via multi-slice spiral CT or MRI enhanced scans. This integration provides a more realistic and accurate representation of cardiac anatomy and spatial relationships.
Furthermore, intracardiac catheters can collect comprehensive intracardiac electrical activity data, which can visually display critical information such as the origin of tachycardia, conduction pathways, reentrant circuits, and slow conduction zones. This facilitates a better understanding of arrhythmia mechanisms and the formulation of catheter ablation strategies.
In recent years, the concept of green electrophysiology has emerged, emphasizing the use of 3D mapping systems and intracardiac ultrasound to achieve electrophysiological studies and catheter ablation with no or minimal radiation exposure.
Cardiac Imaging
Cardiac imaging plays an important role in assessing the relationship between structural and functional abnormalities of the heart and arrhythmias. Echocardiography is the most used imaging modality, including:
- Transthoracic echocardiography (TTE)
- Transesophageal echocardiography (TEE)
- Intracardiac echocardiography (ICE)
TTE is often used to evaluate the relationship between structural and functional abnormalities of the heart and arrhythmias. For example, patients with cardiomyopathies or myocarditis who have ventricular systolic dysfunction and chamber enlargement are more prone to ventricular tachyarrhythmias. Patients with Ebstein anomaly are more likely to develop atrioventricular reentrant tachycardia (AVRT).
ICE involves mounting a miniature ultrasound probe at the tip of a catheter, which is delivered into the heart via peripheral blood vessels (arteries or veins). This technique provides real-time, high-quality imaging of the heart and its adjacent structures, as well as hemodynamic measurements. ICE can directly visualize cardiac anatomy and clarify anatomical relationships between different cardiac structures. It is increasingly being applied in electrophysiology to guide various cardiac interventional procedures.
Additionally, cardiac magnetic resonance imaging (MRI) has become a valuable tool in recent years. It is used to:
Assess myocardial scar burden after myocardial infarction
Detect myocardial fibro-fatty infiltration in patients with arrhythmogenic right ventricular cardiomyopathy (ARVC)
Identify other structural changes that may influence arrhythmia susceptibility
Contrast-enhanced MRI and 18F-fluorodeoxyglucose positron emission tomography-computed tomography (18F-FDG PET-CT) are also used in the diagnosis and treatment response evaluation of cardiac sarcoidosis.
Head-up Tilt Test
The head-up tilt test (HUT) is a commonly used method to evaluate autonomic nervous system function. By changing the patient’s posture, the test redistributes blood volume to the lower extremities under the influence of gravity, triggering neuro-mediated reflex activity that may induce reflex syncope.
A positive HUT result is characterized by:
- A drop in blood pressure (e.g., systolic blood pressure decrease >20-30 mmHg, diastolic blood pressure decrease >10 mmHg)
- A significant reduction in heart rate (<40 bpm) or cardiac arrest lasting >3 seconds
- Reduced cerebral perfusion, leading to presyncope or even loss of consciousness
- In some cases, patients exhibiting an abnormal increase in heart rate (>120 bpm or an increase of >30 bpm)
HUT is commonly used to:
- Diagnose recurrent unexplained syncope
- Differentiate vasovagal syncope from orthostatic hypotension and postural orthostatic tachycardia syndrome (POTS)
Genetic Testing
Genetic testing is often performed for survivors of recurrent malignant arrhythmias or sudden cardiac arrest, as well as for younger patients with a family history of inherited arrhythmias who are strongly suspected of having ion channelopathies.
Ion channelopathies are a diverse group of disorders. Different mutations in the same ion channel may result in varying clinical phenotypes, while the same clinical phenotype may arise from mutations in different ion channels.
Currently, the most well-characterized ion channelopathies include:
- Long QT syndrome (LQTS)
- Short QT syndrome (SQTS)
- Brugada syndrome
- Early repolarization syndrome
- Catecholaminergic polymorphic ventricular tachycardia (CPVT)
- Idiopathic ventricular fibrillation (IVF)
- Hereditary cardiac conduction disorders
- Familial atrial fibrillation (AF)
Genetic testing helps identify potential carriers within families, clarify the genetic defects, and establish genotype-phenotype correlations. It also guides treatment strategies. However, many causative genes for ion channelopathies remain unidentified.
To be continued
Atrial Arrhythmia
Atrioventricular Junctional Arrhythmia
Ventricular Arrhythmia
Cardiac Conduction Block
Interventional and Surgical Treatment of Arrhythmias